Leading Blues Plan Turns Bold Vision
into Business Agility with SmartBPM®
Servicing Backbone
Challenge
Develop a Servicing Backbone that takes
the complexity out of back-office processing
and improves customer experience. Two
incumbent rules engines lacked the power
and the business process management
capabilities needed to manage the constant and
accelerating pace of changes faced by a leading
Blues Plan.
Impact
Creation and extension of a BPM Servicing
Backbone that improves speed to market of
new services and empowers business users
across the enterprise to better meet industry
and customer needs.
Solution
Pegasystems’ SmartBPM technology,
including two focused healthcare solutions —
Pegasystems’ Healthcare Industry Foundation
and Pegasystems’ Claims Repair Solution
Framework — deployed for 13 applications
across five of the Plan’s divisions, creating a
powerful BPM Servicing Backbone.
Benefits
� $20+ Million annual savings
� 40% membership growth and
corresponding revenue attainment in new
product lines
� 75% cycle time reduction for new feature/
program development
� 80% improvement in enrollment
productivity for commercial and
government products
� 97% straight-throughprocessing for HSA
pharmacy claims
A not-for-profit healthcare organization generating several
billion dollars in annual revenue and processing hundreds of
millions of claims per year recognized that a seismic shift was
beginning in the health insurance industry. The regional Blue
Cross and Blue Shield Plan reacted quickly and effectively,
arming itself with game-changing technology and deploying it
across the enterprise as a powerful Servicing Backbone. The
Plan’s speed, innovation and savings improved dramatically
and continue to grow as it further extends its BPM-powered
Backbone across its operations.
The Challenge: Reduce Complexity and Improve Customer
Responsiveness
Rapidly changing industry conditions and a competitive landscape led
the Plan’s Board of Directors to issue a bold strategic imperative: take the
complexity out of back-office processing, speed time to market for new
products and improve customer responsiveness. The resulting vision was
a “Servicing Backbone”: an enterprise-wide framework to handle all types
of business transactions (claims, enrollments, authorizations, billing and
more) — across all lines of business — and all transaction channels (web,
phone, fax, etc.) — in an efficient and technically optimized solution; one that
would cut costs, simplify innovation, and minimize the disruption of change.
But the organization’s existing technical portfolio, including two incumbent
rules engines, was insufficient to execute on the vision. For that, the Plan
needed game-changing technology that would automate the interplay of
business rules and processes; drive transactions through completion; reduce
manual, error-prone activity; and extend easily and intelligently to wherever
needed throughout the enterprise.
The Solution: BPM Technology — Agility in Action
To turn technical vision into reality, the Plan selected
Pegasystems’ award-winning SmartBPM® platform.
Following an extensive evaluation process, the Plan
concluded that SmartBPM aligned best with its vision,
including its goals for improving its ability to self-manage
change by empowering both technical and business staff.
Pegasystems’ software offered unique capabilities such as
intent-driven user portals, change-aware specialization and
built-in re-use capabilities that would help the Plan quickly
achieve advanced business processing. Superior rules and
business process management capabilities, as well as the
maturity and depth of the BPM software and a rich suite
of foundational healthcare solutions, made Pegasystems’
technology uniquely suited to power the Plan’s Servicing
Backbone.
Servicing Backbone Improves Full Range of
Claims Processing
A pioneer in offering Consumer Driven Health (CDHP)
products, the Plan initiated the Servicing Backbone to
optimize Health Saving Account (HSA) claims where
real-time accounting of blended medical and pharmacy
accumulators (such as deductibles and other out-of-pocket
member expenses) is required to correctly pay claims. In the
Plan’s former environment, it took two days to process these
claims because required data resided in multiple systems
and formats. Not having real-time claims payment abilities
resulted in incorrect payments, customer complaints, rework and high processing costs.
For the core of the BPM Backbone, the Plan deployed
Pegasystems’ Healthcare Industry Foundation. Benefiting
from Pegasystems’ pre-packaged industry components,
the Backbone went live in under six months and the Plan
immediately saw dramatic results.
For its maiden deployment, the BPM Backbone drove key
claim processing activity, including claim data assembly
across multiple back-end systems, accumulation validation,
image storing, claim-specific edits, duplicate identification
and group benefits validation. Pegasystems’ BPM software
also provided seamless bi-directional integration to the
Plan’s pharmacy benefit manager (PBM). Multi-system
integration plus the immediate assembly and evaluation of
data enabled real-time claims processing. Within months of
launching its BPM Backbone, the Plan was achieving 97%
straight-through-processing of HSA claims — significantly
driving down disgruntled calls, re-work and other negative
downstream effects of incorrect and untimely claims
Intent-driven user portals
Instantaneously merges business goals with user intent
to optimally tailor each interaction for clarity, content
and suitability.
Change-aware specialization
Automatically invokes the right rule at the right
time based on business-specific variables including
customer, product, channel and line of business.
Re-use capabilities
Simplifies sharing of enterprise best-practices and
common rules. You declare only the differences rather
than duplicating policies and procedures in multiple
places and multiple versions.
payment. This initial Backbone deployment also included an
integrated desktop for claims operators to streamline and
improve quality in processing pended claims.
Ultimately the BPM Backbone was expanded to four
additional claims areas including a solution for Medicare
adjustments where the BPM Backbone automates
correspondence and literature fulfillment, applies error
edits, and drives business processes to move operators down
one of 27 distinct adjustment paths based on the specific
processing rules. The Backbone was also extended to handle
the correction of National Provider Identifier (NPI) errors,
by guiding users through pertinent processes via tailored
portals, for quicker, high-quality service and improved
compliance with federal regulations. The Plan later added
Pegasystems’ Claims Repair Solution Framework to the
Backbone to rapidly meet new Blues Association claims
mandates aimed at improving provider servicing. The Plan
now runs all its claims through the BPM Backbone — over
300 million transactions annually — for automated preadjudication and post-adjudication processing.
BPM Delivers Agile Framework for Change
Across the Enterprise
Today, the BPM Servicing Backbone has exceeded the Plan’s
original vision and is supporting 13 applications across
five Plan divisions. Advancing quickly from departmental
solution into an enterprise-wide implementation, the BPM
Backbone now supports the work of more than 30% of the
organization’s employees across the functions of claims,
enrollment, finance, health management and benefits.
For benefits, the BPM Backbone is used to streamline
complex benefits categorization functions and facilitate faster
product roll-outs. The Backbone provides business users
with re-usable, stackable components containing benefit
product information for various product lines. This centralized
process provides real-time access to benefit information
and a simple user interface to construct, edit, and save
business benefit components in a persistent database. These
components are then re-used to build even more complex
benefit components and feed integration engines to provide
the information in downstream system formats.
Another deployment applies the Backbone to the Plan’s
incentive-based benefits products. In this application, the
Backbone utilizes Pegasystems’ integrated BRE (Business
Rules Engine) functionality in a stateless manner to return
scores for incentives, ranging from gift cards to actual check
payments, based on complicated logic including health
and wellness activities completed by the member. Built
expressly for high throughput, this portion of the Backbone’s
functionality has achieved sustained rates of more than
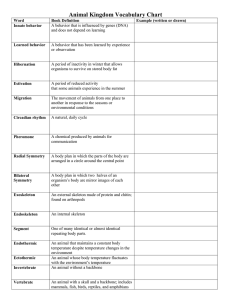
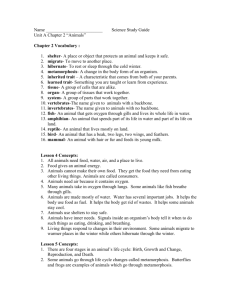
Membership
Underwriting
Commissions
10,000 transactions per hour. What began as a new product
feature for a major long-term customer has now been
extended to additional clients eager for program offerings
that focus on wellness and foster member loyalty.
Pegasystems-Powered Backbone Drives $20
Million in Annual Savings
Sound design, game-changing software and thoughtful
execution created a robust foundation that supports a new
rhythm for change and for deployment. As the Servicing
Backbone was extended and the Plan increased its number of
avid users, the organization focused on business enablement
and the ease of extension. The Plan’s BPM initiatives
increasingly provided business users with opportunities
and vehicles to make their own changes — whether this
involved updating activities, setting new properties, modifying
decision tables or managing decision and routing rules. The
Plan formalized the intersection of its Business and Rules
organizations and created its own “Cookbooks” for optimal
re-use and design. In 2009, the Plan was awarded honorable
Adjudication
Platform
Finance
SAP
Letter
Generation
SmartBPM Servicing Backbone
Benefits
• Benefits
Categorization
Enrollment
• Individual
Products
Enrollment
• Enrollment
Exceptions
Claims
• Accumulators
for HSA Claims
• Medicare
Adjustments
• NPI Exceptions
• BCBS
Association
Mandates
• Prompt Pay
Mandates
• Pre- & Postadjudication
Repair
Health
Management
• Incentive Based
Benefits
• ID Stratification
Finance
• Claims Cash
Management
• Medicare
Payment
Reconciliation
• 13 applications across five divisions & multiple channels (web self-service & broker sites)
• Over 300 million annual transactions (entire claims volume); sustained rates of 10,000/hr
• Over 1,000+ internal users; thousands more external users
mention for “Best BPM Bottom Line” from a prestigious
technology research firm.
In less than three years, Pegasystems’ SmartBPM has
become the Plan’s true backbone; a robust and powerful
technology platform, improving transactions and business
processes across the organization. Today, the BPM
Backbone even does disease management functions
such as ID stratification to identify care management
program candidates and it also optimizes the Plan’s cash
flow and maximizes revenue through intelligent claims
cash management and automated Medicare payment
reconciliation functionality.
Turning vision into reality, Pegasystems SmartBPM has
enabled extensive automation, re-use of processes and highly
consistent transaction processing for the Plan. Perhaps the
most compelling evidence of Pegasystems’ value is the Plan’s
realization of $20 Million savings annually; savings which
are expected to grow even larger as the Servicing Backbone
continues to drive improvements across the rest of the Plan.
The Vice President, Business Design and Enterprise
Transactions said, “We take compliance seriously, and
we have committed significant resources and technology
to ensuring that we are taking the right approach. We’ve
recently expanded the platform that supports our compliance
efforts into the revenue cycle, uncovering potential errors at
a rate quicker than ever. For example, in one month alone
we were able to sift through 26,000 entries in real-time, with
corrections made on-the-fly.”
Expanding the Servicing Backbone to
Maximize Revenue Growth
Due to its enormous success in providing new efficiencies
and slashing costs, the Servicing Backbone was quickly
turned to customer acquisition initiatives to speed
enrollment and maximize membership growth opportunities.
To streamline enrollment, the BPM Backbone was used to
create re-usable data entry forms, exception screens and
workflow across multiple business areas. Functionality
includes a common interface for incoming electronic
application data; automation of data services for business
rules, data access and system integration; automation of key
business rules such as validation, routing and data set-up;
and the automation of membership transactions into the
Plan’s back-end systems. The functionality is applied to
multiple product lines, including individual and Medicare
offerings and is used across numerous channels including
Direct-to-Consumer portals, broker Web sites, centralized
e-shopping organizations and more.
By eliminating redundant data entry and multiple, manual
business handoffs, the customer acquisition-focused
components of the Servicing Backbone have improved sales
cycle times, minimized staff additions, and provided the Plan
with agility to shift resources where most needed. Prior to
the Servicing Backbone’s deployment, several products’
enrollment process were entirely manual; one had daily
average inventories of more than 200 applications, with five
days of work on hand. With the Servicing Backbone, the Plan
boosted productivity by 80% and quickly attained a 50% clean
first-pass rate for automated enrollments. Membership ID
Cards reached enrollees quickly, vastly improving members’
enrollment experience. Along with increased productivity,
improved visibility into application status and reduced
training times, the Blues plan also credits its BPM Backbone
for a 40% membership gain in new products and the revenue
that corresponds with that growth.
“The flexibility offered by Pegasystems’ rulesdriven BPM platform is helping us create agile
solutions to best meet our customers’ needs; it’s
keeping us nimble so we can continue to succeed
in the increasingly changeable healthcare
environment.”
Vice President
Business Design & Enterprise Transactions
Regional Blue Cross and Blue Shield Plan
For more information, please contact your Pegasystems representative, visit us on the Web at www.pega.com, or email us at
info@pega.com. © Copyright 2010 Pegasystems. All rights reserved.