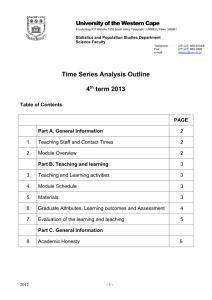
Unit 2 - University of the Western Cape
advertisement

UNIT Understanding Disease 2 Introduction Because of the advances of medical knowledge, the medical school curriculum has become so crowded that the social importance of preventive medicine and public health is seldom emphasized. This creates a blind spot which often persists throughout professional life and results at times in misunderstandings between the practicing physicians and the constituted health authorities of the community. (Miller, Baehr & Corwin, 1942.) I wonder how many of you agree with this statement – that physicians and Public Health authorities sometimes do not see eye to eye? It may even have motivated you to embark on a professional degree in Public Health. Addressing that “blind spot” is our main motivation in this programme, but in addition, you need to ensure that you have a strong basis for undertaking disease prevention. Miller, Baehr and Corwin (1942) were motivating to draw clinicians and the Public Health professionals closer together, but they also suggest an important dimension of this unit – that disease prevention requires a different perspective. This is what this Unit will try to do – to shift your perspective on different classes of disease to a preventive vision. This requires you to have involves a thorough basis for understanding diseases themselves - the different kinds of diseases including diseases which are infectious or communicable, the rising tide of noncommunicable diseases, and the very real presence in Lower and Middle Income countries of ill health arising from injuries - their natural history and etiology. This sounds like a tall order, but it is more a call to for acquainting yourself with key principles of the spread and control of different classes of disease and knowing where to find more information when you need it. Etiology (alternatively aetiology) is the study of causation, or origination. Aetiology (2nd ed. ed.). Oxford University Press. 2002. Some aspects of this Unit will constitute revision for many of you, but at the same time, will be looking at disease at population level. You, as a Public Health professional need both the basic skills of an epidemiologist and the in-depth knowledge of disease of a clinician because in order to address and respond to disease, you need to understand a number of dimensions of a disease. This includes what we call its biological basis, and it involves its natural history, how it is spread, its risk factors, and its effects on the human body. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 53 At the same time, a Public Health professional looks at disease from a “helicopter position” overseeing the health of populations, and therefore needs to be able to read measurements of the extent of ill health or disease, and monitors the growth and trends of diseases. Study Sessions There are five Study Sessions in Unit 2. Study Session 1 Introduction to disease Study Session 2 Populations and health Study Session 3 Communicable diseases Study Session 4 Non-communicable diseases Study Session 5 Injuries and violence In the course of this unit, you will be encouraged to read texts and do a range of tasks that will lead to your achieving these outcomes: Intended Learning Outcomes By the end of this unit you should be able to: Health Measurement Outcomes Deepen and strengthen knowledge and understanding of disease, injuries and violence Understand concepts and classifications of disease Understand, measure and analyse communicable and noncommunicable disease in different sectors of the population Identify international, national and local sources of information on health and diseases in populations Academic Learning Outcomes Employ critical reading skills to a range of academic and health related texts and datasets Employ higher level numeracy skills for practice in the field Read and analyse a range of data, graphs and diagrams Develop research skills using the Internet and a range of academic and local sources Apply academic referencing skills Organise own programme of study SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 54 Unit 2 - Session 1 Introducing disease Introduction We have already spoken about definitions of health in Unit 1 and you may remember the WHO definition of health - “Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” (WHO, 1948). A critical aspect of this definition is that it does not limit health to absence of disease but rather focuses on the positive concept of well-being. Additionally, the definition includes the mental and social states too, and over the years the definition has been expanded to include spiritual and emotional health. Whilst there is general agreement that this is an ideal to be attained, one of the criticisms levelled at the definition is the difficulty of defining and measuring “wellbeing”. So, in practice we often still define health by the presence or absence of disease. In this session, you are reminded of or introduced to the ways in which disease is measured. Contents 1 2 3 4 5 6 7 Learning outcomes of this session Readings Disease description and measurement Broad classification of diseases Sources of information for health Session summary References and further reading SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 55 1 LEARNING OUTCOMES FOR THIS SESSION By the end of this unit you should be able to: Health Measurement Outcomes Academic Learning Outcomes Apply and explain common measures of health and disease in Public Health Demonstrate familiarity with international, national and local sources of information on health and diseases in populations Demonstrate familiarity with key concepts for describing the broad groups and classifications of disease Identify sources of health information 2 Identify and locate sources of information Read and interpret graphical representations Employ higher level numeracy skills for practice in the field READINGS AND REFERENCES The readings for this session are listed below. You will be directed to them in the course of the session. Author/s Lucas, A. O. & Gilles, H. M. Publication details (2003). Ch 2 – Health Statistics: Information for Health. Short Textbook of Public Health Medicine For the Tropics. 4th ed. London: Arnold Publishers: 11–28. (See prescribed setwork) Birn, A-E., Pillay, Y. & Holtz, T. H. (2009). Ch 5 – What Do We Know, What Do We Need to Know, and Why it Matters – Data on Health. Textbook of International Health: Global Health in a Dynamic World. New York/ Oxford: OUP: 192–224. Vaughan, J. P. & Morrow, R. H. (1989) Ch 14 – Epidemiological Principles. Manual of Epidemiology for District Health Management. Geneva: WHO: 17–20. (See prescribed setwork) SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 56 3 DISEASE DESCRIPTION AND MEASUREMENT 3.1 Describing disease in populations One of the first lessons in describing population-wide health is to recognise that there are conventions for doing so, and that specificity is required at all times. By saying this we mean that any health measurement should be expressed in terms of time, place and persons, i.e. when they occur, where they occur and in whom they occur. With regard to time, outbreaks are described in terms of days or weeks. Some diseases are seasonal and should be described accordingly. Epidemics such as HIV/AIDS data should be monitored annually to allow for regular adjustment of plans and services. As far as place is concerned, it is essential to recognise that disease patterns vary by country and region at international, national and local levels. Data that is presented without reference to location of origin is meaningless. Finally, in describing who is affected, age, sex, socio-economic group, occupation, ethnic origins are just some of the variables that are used. This is important because some groups are more susceptible to particular diseases than others. So make it a practice to always be precise when presenting data. Include information on time, place and who is affected. Here is an example: More than 20 million infants worldwide are born with low birth weight, of which 16.5% are in developing countries and 7% in developed countries (UNICEF & WHO, 2004). A review of data from the Katutura Hospital information system revealed that the rate of low birth weight in the Khomas region of Namibia for 2006 was 17.4% in 2006. 3.2 Measuring disease frequency As was said in Unit 1, Public Health focuses on populations, rather than individuals. “The assessment of the health of an individual is usually made … by taking a medical history, doing a physical examination, laboratory tests and other special investigations” (Lucas & Gilles, 2003: 11). Theoretically, the health of a whole community could be defined by assessing each individual in this way. This would of course be rather cumbersome and time-consuming. In practice, the health status of a population is assessed indirectly by collection and interpretation of important events that serve as indicators of the health of the community, such as death (mortality data) and sickness (morbidity data). Professionals in the field of Public Health work with epidemiological tools to “study the distribution, frequency and determinants of health problems and disease in human populations” (Vaughan and Morrow, 1989: 9). So part of epidemiology is describing the frequency of health problems or disease in the population. By frequency we simply mean how many times an event occurs within a specified period. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 57 Disease frequency can be measured in a number of ways. Data can be provided as absolute numbers or counts. Information can also be stated as a ratio or proportion. However, the most common way that data is presented is as a rate. 3.2.1 Absolute numbers or counts The most readily available data is usually in absolute numbers (e.g. 12 adults) or counts; these are useful in reporting and monitoring infectious diseases, especially outbreaks when the population involved is restricted in time and locality, and the population structure is stable. For example, in late 2009, … three cases of measles were confirmed in the Engela District in the north of Namibia, while the Ministry of Health and Social Services [was] investigating 21 more suspected cases. (The Namibian. Windhoek, 25 November 2009) Clearly the Ministry feels that even this relatively small number of cases is an important Public Health issue and one which should be investigated, monitored and addressed if necessary. The reasons for their concern could be because children in this population are at risk on account of low immunity, caused for example by their poor nutritional or HIV status. The response of the Ministry to new infections generally depends on: the size and context of the population, e.g. a community with a high proportion of vulnerable young children or a children’s hostel would draw a more urgent response. the infectiousness and severity of the disease, e.g. cholera, H1 N1 virus or even a single case of Ebola virus would affect an urgent response. You’ll be learning more about communicable diseases in Session 3 of this Unit and more about outbreaks in the module on Descriptive Epidemiology. The main purpose of this Study Session is to cover the different ways that health and disease can be measured. Although absolute numbers are likely to be the most accessible data in an outbreak, they do not tell us the severity of the problem, nor allow comparison of the frequency of the problem in different groups or over time. For example in the Namibian measles example, we do not know what proportion of the population is infected, and therefore we do not know whether it constitutes an epidemic, i.e. a higher proportion of the population than is usually expected. However, we still rely on absolute numbers when it comes to allocation of health resources, e.g. how many people in the population in relation to the provision of vaccinations. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 58 3.2.2 Ratios Health measurement may also be undertaken in ratios, for example, you may want to know how many of those affected by measles are male. Males (x) Males (x) Females (y) All those infected (y) (a) (b) The variables, or differing features, are labelled x and y. The values of x and y may be completely independent, as in (a) above, or x may be included in y, as in (b) above. Example (a) above is an example of a ratio. Ratios are expressed as follows: 7 males to 10 females or 7:10 with a colon between the variables. A measurement of 50 males to 100 females would be reduced to a ratio of 5:10 and then further reduced to a ratio of 1:2. 3.2.3 Proportion In many situations, however, we want to determine the magnitude of the problem and in order to do this we need to know the size of the problem in relation to the population at risk of contracting the disease. If we had this information, it would help us to assess the seriousness of the problem of measles in Engela District and maybe compare it with that in another district. Where x is part of y, the frequency measure is called a proportion. In the example above, only (b) is a proportion, as the males are a proportional part of the whole population of those affected by measles. In (a), males are not a proportional part of females. In the Engela District, those with measles are a proportion of the population. 3.2.4 Rates In Public Health reporting generally, it is most common to report information as a rate of the population affected by a disease. Although they serve a similar purpose to proportions, rates have the added dimension of time: they measure the occurrence of an event in a population over time (Centres for Disease Control, n.d). Rates “... relate the number of cases to the size of the population at risk in the specified group in the specified period” (Joubert & Ehrlich, 2007: 20). A rate differs from a proportion in that it involves a measure of time. “A rate is calculated by dividing the number of cases (numerator) by the population at risk and the period of observation (denominator). Rates express the frequency of some characteristics per 1 000 (or 10 000 or 100 000) persons of the population per unit of time” (Joubert & Ehrlich, 2007: 21). The SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 59 components of a rate are a numerator and a denominator. The numerator is a sub-part of the denominator. If there are three cases of measles in the under-5 population (numerator) of the population of 500 at risk in one year, the disease rate is: numerator (a sub-part of the denominator or population) denominator (the population at risk) } } 3 = 6 per 1 000 500 x 1 year i.e. The number of cases or events occurring during a given time period x 10n Rate = population at risk during the same time period The population at risk refers to the group of people who have the potential to get the disease and may contribute to the total number of cases. It may refer to the whole population in a district or country or all people of a particular age group. It is also called the denominator population. There are three important aspects of this formula. The persons in the denominator must reflect the population from which the cases in the numerator arose. The counts in the numerator and denominator should cover the same time period. In theory, the persons in the denominator must be “at risk” for the event, that is, it should have been possible for them to experience the event. (Centres for Disease Control, n.d.) So a rate for the Engela example would be calculated as follows: numerator (a sub-part of the denominator or population) denominator (the population at risk) } } The number of measles infection occurrences in children under-5 The population under-5 at risk in Engela during a fixed period TASK 1 – What data is needed to calculate rates? Read the rest of the newspaper article on the measles outbreak in Namibia and then answer the questions that follow. In the same report from The Namibian, it is noted: At a meeting of the National Health Emergency Management Committee (NHEMC) on Tuesday, Primus Shilunga, Acting Deputy Director in the Epidemiology and Disease Surveillance Directorate, confirmed that an outbreak of measles in Angola was starting to make SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 60 its way into Namibia. Of the 21 suspected cases that have been reported at villages in the Engela District, 12 of the patients are Angolan citizens, and nine are Namibians. A suspected case of measles in a 24-year-old man has also been reported in Okuryangava in Windhoek. Shilunga said that in Angola's Kunene province, at Oshikango, 12 cases of measles have been confirmed, and 67 suspected cases presented. He said although measles usually infects children under the age of five, the mean age of those suspected and infected is 13.4, with 61 per cent of the cases being over the age of five. Only two of the suspected cases are under the age of one. The Ministry's routine vaccination drive, of which one campaign was recently concluded, covers children under the age of one. Shilunga said the older age infection trend is a cause of concern, as there is a higher risk of complications for older people who have not been vaccinated. Possible complications include diarrhoea, pneumonia, encephalitis (inflammation of the brain), and conjunctivitis (commonly called 'pink eye') or even blindness. (The Namibian, 25 November 2009) 1. Why do you think the data in this newspaper article is given as absolute numbers? 2. What proportions are provided by the report? Are they rates and why or why not? 3. What is the significance of these proportions in addressing the problem? FEEDBACK 1. It is likely that absolute numbers are given because this is the only information that is available. It is also an early stage in the outbreak, and the Department concerned is still monitoring the situation. They may also not have population data for the district, and besides they may be unsure which age group data to focus on, as the outbreak is taking place across a wide age range, but particularly amongst teenagers and in adults rather than amongst under-5 infants. 2. The proportions which are provided are the proportions of infected children divided into age groups. Out of the total number of measles cases, the proportion of cases of measles in children over-5 years is 61% and therefore the Mean Another measure you will come across here and elsewhere is a mean age. The mean is the same as the average. It is calculated by adding all the values together and dividing the total by the number of people in the sample. In other words, all ages of infected peoples would be added together, and divided by the number of people, e.g. for a group of 5 SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 61 proportion of cases in those under-5 years will be 39%. This is important because measles most commonly occurs in children under-5 years of age. These proportions are not rates because they are not measured over time. 3. The significance of the proportions is that they highlight which age group has been affected, and this alerts the health professionals to whether they are more or less at risk. (The report states that the mean age of cases is 13.4 years and that there is a higher risk of complications in this age group). Look at pages 17–19 of your setwork by Lucas and Gilles (2004). This has a short introduction to rates. READING Lucas, A. O. & Gilles, H. M. (2003). Ch 2 – Health Statistics: Information for Health. (2003). Short Textbook of Public Health Medicine For the Tropics. 4th ed. London: Arnold Publishers: 17–19. Illustration of rates using the IMR To illustrate the concept of rates, the IMR example below demonstrates the necessary features. As you now know, an IMR or Infant Mortality Rate is the number of infant deaths under 1 year during one year divided by the number of live births during the same year X 1 000. Here the time dimension of the rate has been underlined. For example, the IMR for Khayelitsha in 2000 was 47/1 000. The IMR is a standardized rate and has come to be used as an approximation of the health status of a whole population because a high IMR usually signifies lack of services, poor infrastructure and impoverished living circumstances. Take a look at this bar chart or histogram below representing the Infant Mortality Rates (IMR) from 2000 measured by municipality for Cape Town, South Africa. Each bar represents a different municipal area of the city, and the length of each bar represents the rate per 1 000 or frequency of infant deaths. The chart demonstrates the impact of economic and social disparities between some of the most affluent suburbs of Cape Town – Central and SPM (South Peninsula Municipality) and the most economically deprived, Nyanga and Khayelitsha. This illustrates how IMR serves as a helpful Public Health measure drawing attention to where resources should be allocated. NOTE: IMR or Infant Mortality Rate is the number of infant deaths under-1 year during one year divided by the number of live births during the same year X 1 000. IMR Please take note of the precision of this rate or standardized indicator which has a universally agreed definition. The convention is to give this rate as a proportion of 1 000. This is because a percentage or proportion of 100 would be very small, 0.045 for example, which is less understandable because we relate to whole person numbers and not fractions of persons. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 62 Infant Mortality Rate (IMR) 50 40 30 20 10 Region Tyg. West Tyg. East SPM Oostenberg Nyanga Mitchells Plain Khayelitsha Helderberg Central Blaauwberg Athlone 0 Until 1994, the South African population was segregated by “race” and economic class. These socio-economic factors have impacted on health, as seen through this indicator graph. Nyanga and Khayelitsha were designated residential areas for black people and were deliberately under-resourced during apartheid. Khayelitsha is a newer suburb, which has grown rapidly since the 1990s. Oostenberg includes many of the historically “coloured” areas, and is on the fringes of the city. Source: Cape Town Equity Gauge, SOPH, UWC, 2004 3.3 Vital statistics The starting point for health measurement is routinely available information, and the main source of health measurement has remained death statistics. Health information is useful for planning, implementing and evaluating health services. Vital statistics are the data obtained through registering “vital events – births, deaths, marriages and divorces” (Lucas & Gilles, 2003: 11). Historically, it is mortality data that has remained the main source of “health” statistics, and although considered a narrow way of looking at health, mortality statistics offer a window on the health disparities between poor and more affluent communities.” (Beaglehole & Bonita, 1997). Statistics is the science of summarising and analysing data that are subject to random variation (Last, 1999). SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 63 Many developed countries have compiled statistics of mortality and morbidity for many years through collection of vital statistics from birth and death registrations and from surveillance systems and surveys. However in many developing countries even information on mortality is not available due to lack of reliable systems to collect vital statistics. 3.3.1 Mortality Data The most substantial source of mortality information is data provided to the WHO by member countries, although “… only 60 of the 187 member states are in a position to provide national death statistics …” (Beaglehole & Bonita, 1997: 4). The availability of such data is related to “an absence of national death registration systems for two third’s of the world’s population …” and in consequence, estimates are often used (Beaglehole & Bonita, 1997: 4). Two elements are essential for mortality statistics to be useful: one needs to know the size of the population who are at risk; one needs to identify deaths (Beaglehole & Bonita, 1997: 4) (that is gather data). Beaglehole and Bonita (1997) summarise the purposes for which mortality data is used. In their words, they: Allow comparisons among and within countries; Demonstrate trends in longevity or life expectancy; Show trends in death rates for different age groups; and Provide information about the leading causes of death (Beaglehole & Bonita, 1997: 5). Accurate mortality data is a priority for every country, and yet the quality of mortality data is sometimes compromised by factors such as changes in death certification styles, revision of disease classification systems, classification difficulties with multiple causes of death, e.g. for AIDS patients, lack of routine registers, the exclusion of poorer communities and the decline in use of post-mortems (Beaglehole & Bonita, 1997: 5; Joubert & Ehrlich, 2007). For coding the cause of death, standard procedures have been established known as The International Statistical Classification of Diseases and Related Problems. In many countries, however, mortality data may be unreliable. READING Birn, A-E., Pillay, Y & Holtz, T. H. (2009). Ch 5 – What Do We Know, What Do We Need to Know, and Why it Matters – Data on Health. Textbook of International Health: Global Health in a Dynamic World. New York/Oxford: OUP: 210–224. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 64 TASK 2 – Find out about mortality data Explore the extract on vital records and mortality data from Birn, Pillay and Holtz (2009) pages 210–224 with these questions in mind: 1. Identify four different ways in which vital statistics are used. 2. Are there disparities in the quality and availability of birth records worldwide? If so why? 3. Try to find the website address (url) for the Demographic and Health Survey. Find demographic and health data and survey information for your own country or for a neighbouring country. When was the last survey for that country compiled? What else in this site could be useful to you? 4. Why does mortality data constitute a key source of data for health assessment and planning? 5. What are the processes between a death and its registration in a national database? 6. What is the denominator of the IMR? 7. In which region has the IMR increased and during what period? 8. Why is IMR data often unreliable? 9. Which three countries had the highest IMR in 2006, and which the lowest? 10. Two rates are regarded as indicative of the health status of a country at international level. What are they? FEEDBACK Here are a few of the more difficult answers to check yours against: 3. The url is http://www.measuredhs.com/ The last time a Demographic and Health Survey was conducted in South Africa was 2003-4. The HIV/AIDS Survey Indicators Database looked interesting and provides an easily accessible comprehensive source of information on HIV/AIDS indicators derived from sample surveys. 4. Mortality data has always been regarded as a key source because they are inherently unambiguous because death is an absolute state; however, this is not so with regard to cause of death; mortality data is also a key source because it is more frequently kept on a larger scale than other data. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 65 6. The denominator of the IMR is the number of live births in a country during a year. This differs from other denominators because they are derived from registration data and not census estimates. READING TIP: Note that reading comprehension and focus is enhanced by reading a text with questions in mind. Whatever you read, pre-read the text and try to formulate some topics you are searching for information about, or even some questions to answer. 3.4 Crude or specific rates Death rates are calculated as crude death rates. “If the total number of cases in a population is divided by the size of the population at risk, a crude (or overall) rate is calculated (Joubert & Ehrlich, 2007: 23). This rate makes no reference to cause or age group – hence the word crude. “If the epidemiologist is more interested in what the rates are for subgroups, for example, for the sexes or for different age groups … [t]hese are called specific rates … e.g. heart disease mortality rates for men in the 55 – 64 year age group” (Joubert & Ehrlich, 2007: 23). To calculate the crude mortality rate you divide the number of deaths in a given year by the average whole population in the same year and multiply by 1 000. Number of all deaths in a given year Crude mortality rates = X 1 000 Average whole population during same year Crude rates are also calculated for births. The main disadvantage of crude rates, however, is that they do not take account of the influence of multiple factors on mortality, such as age, sex or socio-economic class. So far we have only discussed the measurement of mortality, but the innovation of the first Global Burden of Disease Study (GBD) changed this by developing the means to quantify ill health (morbidity) and its impact on society. This enabled us to gain a more comprehensive picture of the health of communities and nations, particularly in the age of non-communicable disease growth. The new measures to calculate morbidity will be discussed later in the context of the Global Burden of Disease study in Study Session 2. 3.5 Health indicators You have already encountered the IMR and been introduced to the idea that it is used as a way of exposing or “indicating” the health status of a whole population. The IMR is just one of a set of rates known as health indicators and defined as ”… a measure that reflects or indicates the state of health of persons in a defined population. This could be the total population or part of the population, e.g. infant mortality rate.” (Vaughan & Morrow, 1989: 160.) SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 66 Indicators are useful to country, or even district health departments to describe the health situation. They can also be used to measure changes over time and monitor progress towards goals such as the Millennium Development Goals (MDGs). For example, this comparison tells a significant story about health trends in these two neighbouring sub-Saharan countries. Year 1960 Zambia 126/1 000 Zimbabwe 109/1 000 1996 112/1 000 49/ 1 000 TASK 3 – Get to grips with health indicators Read pages 17–20 of the reading, your setwork for Descriptive Epidemiology and then answer the questions below. READING Vaughan, J. P. & Morrow, R. H. (1989). Ch 14 – Epidemiological Principles. Manual of Epidemiology for District Health Management. Geneva: WHO: 17–20. 1. How are health indicators used? 2. IMR is said to be an “indirect measure”. What other indicators serve as indirect indicators of population health? What do direct measures indicate? 3. From what sources are indicators derived? 4. What key areas do health status indicators cover? 5. How do you think indicators are developed? You need to use your imagination on this one. FEEDBACK 1. “To analyse a situation Make comparisons Measure changes over time.” (Vaughan & Morrow, 1989: 17) Health indicators are used in health services planning, management and evaluation. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 67 2. The IMR measures the number of children at risk of dying but also indirectly shows the socio-economic status of the population. Indicators derived from mortality rates provide a good picture of population health. Other indirect indicators are: nutritional indicators which provide a picture of the quality of life in a population; overall life expectancy at birth. 3. Indicators are derived from death registrations if a country has reliable death registration information; if not, they can be estimated from surveys, population censuses and other sources. 4. Health status indicators cover nutritional status, morbidity, mortality, fertility, IMR, maternal mortality rate (MMR) and life expectancy at birth. 5. Take a look at page 18 in the setwork which provides some of the most important (key) indicators which you will find used regularly in the literature and which are used in reporting the health status of a population. READING Lucas, A. O. & Gilles, H. M. (2003). Ch 2 – Health Statistics: Information for Health. Short Textbook of Public Health Medicine For the Tropics. 4th ed. London: Arnold Publishers: 18. Take note of the conventions used, e.g. that birth, death, IMR and fertility rates are calculated per 1 000, while maternal mortality rate is calculated out of 10 000. TASK 4 – Practise using these concepts Write out a clear definition of each of these indicators for yourself. You will find definitions in a good medical dictionary or in your copy of Vaughan & Morrow (1989). 1. Fertility rate 2. Nutritional status 3. Infant mortality rate 4. Under 5 mortality rate 5. Maternal mortality rate 6. Life expectancy at birth 7. Using Gilles & Lucas (2003: 18), answer these questions, designed to familiarize you with these indicators: a) What is the denominator for the maternal mortality rate? b) Seven people contracted H1N1 in Region X out of a population of 14 000. Can SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 68 you work out a rate with this data? c) Is the population at risk the denominator or the numerator? d) The numerator is part of the denominator in most cases, but not in the case of the ... rate because ... [complete the sentence]. e) What is the age range for perinatal mortalities? f) What is the age range for the IMR? g) What is the neonatal mortality age range? h) What is the age range of women counted in the fertility rate? i) What is the opposite of a crude mortality rate? j) Why do you think the maternal mortality rate (MMR) is calculated out of 10 000 and not 1 000? FEEDBACK You’ll be disappointed to hear that you should check your answers against the reading because they are too straightforward to provide, except for question j). j) The MMR is calculated out of 10 000 because we cannot conceive of people in fractions or decimals; therefore we convert them to whole numbers by multiplying by 100 (which produces a percentage), or by 1 000 or 10 000 (which then produces a value per 1 000 or per 10 000). We now move on to two important concepts which you will use frequently in the future, so take particular note of them. 3.6 Prevalence and incidence rates In the Namibian measles case example above, we do not know the size of the population or indeed the extent of the problem - we only know the number of cases. In Public Health, however, rates are usually provided to demonstrate what proportion of the population at risk suffers from this condition. If we had an understanding of the number of children and adults with measles in relation to the population size (or number at risk of infection with measles) at a specific time, this would be called the prevalence rate. If we knew how many infants in this population were under-5 years of age, we could also work out the under-5 prevalence rate. The two most common ways to express population health problems or disease frequency are prevalence, and incidence. It is important to note that these are two different measures and they are not interchangeable. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 69 Prevalence Incidence Prevalence is the total number of existing cases or events or conditions in a defined population at a particular point in time (Vaughan, & Morrow, 1989: 164). Prevalence provides a snapshot of the disease in a population (Walley, Wright & Hubley, 2001: 25). Incidence is the number of new cases or events or attendances occurring in a defined population over a defined period of time, commonly one year (Vaughan, & Morrow, 1989: 161). Prevalence is most useful to measure a diseases with a long duration that is, chronic diseases such as hypertension, diabetes, asthma (non-communicable diseases most commonly fall into this bracket) but also communicable diseases like HIV/AIDS and leprosy. Incidence is most useful for diseases with a short duration like diarrhoea, measles, pneumonia – these are mostly communicable diseases. Numerator = all cases Numerator = new cases Denominator = total population at risk of being a case Denominator = healthy population at risk at start of time period (cumulative incidence) OR Sum of disease-free persons at time of observation (incidence rate) Measured over a specific time period Measured at a point in time (Source: Joubert & Ehrlich, 2007: 23) 3.6.1 Calculate prevalence and incidence rates Existing cases at particular point in time Prevalence rate = X factor Total population at risk New cases in a specified period of time Incidence rate = X factor Total population at risk Please note, however, that incidence and prevalence can be presented either as whole numbers or as a calculated rate. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 70 TASK 5 – Distinguish between prevalence and incidence rates 1. To familiarize yourself with these terms, study this example: District A reported 600 new cases of TB in past year; District B reported 400 new cases of TB in past year; Can you say which district faces the more serious TB problem? Why do you say so? 2. It is 2007, and the IMR in your country is 75 per 1 000 total live births. When you compare your district statistics, you note that in 2007 there were 14 000 births, and 1 148 deaths of children under 1 year. Is the problem greater in your district or nationally? FEEDBACK 1. Firstly, let’s see which district has the most new TB cases: obviously it is District A, with an incidence of 600 cases, i.e. 600 new cases. However, to compare the seriousness of the situation, we need to know the population at risk. Now we find that the population of District A is 800 000 and District B is only 200 000. This allows us to calculate the TB incidence rate. The TB incidence rate for District A is: 600 cases/800 000 population = 0.75 cases per 1 000 people The TB incidence rate for District B is: 400 cases/200 000 population = 2.0 cases per 1 000 people So what we see is that the rate in District B, i.e. the proportion infected relative to the population at risk is higher in District B. We then realize that although there were more new TB cases in District A in the past year, TB is actually more common in District B because there are more cases per head of population. You will practice doing your own calculations in your Descriptive Epidemiology module. 2. Your district has less of a problem – the prevalence is calculated by dividing the number of deaths by the total population of your district. This is: 1 148/14 000 x 1 000 = 82 per total live births Be sure to distinguish these two terms from now on and to use them accurately. Early history of disease classification Sir George Knibbs, the eminent Australian statistician, credited François Bossier de Lacroix (1706-1777), better known as Sauvages, with the first attempt to classify diseases systematically (10). Sauvages' comprehensive treatise was published under the title Nosologia methodica. A contemporary of Sauvages was the great methodologist Linnaeus (1707–1778), one of whose treatises was entitled Genera morborum. At the beginning of the 19th century, the classification of disease in most SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 71 general use was one by William Cullen (1710-1790), of Edinburgh, which was published in 1785 under the title Synopsis nosologiae methodicae. For all practical purposes, however, the statistical study of disease began a century earlier with the work of John Graunt on the London Bills of Mortality. The kind of classification envisaged by this pioneer is exemplified by his attempt to estimate the proportion of liveborn children who died before reaching the age of six years, no records of age at death being available. He took all deaths classed as thrush, convulsions, rickets, teeth and worms, abortives, chrysomes, infants, livergrown, and overlaid and added to them half the deaths classed as smallpox, swinepox, measles and worms without convulsions. Despite the crudity of this classification his estimate of a 36% mortality rate before the age of six years appears from later evidence to have been a good one. (WHO. ICD website, [Online], Available: http://www.who.int/classifications/icd/en downloaded 17 1 10) 4 BROAD CLASSIFICATION OF DISEASES How do you think or talk about the different diseases and sources of ill-health? Do you categorize them by cause or do you group them according to their evolution in the human body or perhaps according to the organ they affect? You are sure to have read a number of books on diseases and studied some of them in great detail. Yet since the 19th century, the period when scientists engaged in the mammoth task of organising the world’s scientific knowledge into categories and classifications, there has been a system in place which is used in a number of contexts – this system plays a diagnostic role for medical doctors and medical insurance companies, but primarily it plays a helpful part in the field of Public Health for epidemiologist. It is called the International Classification of Diseases or ICD. 4.1 International Classification of Diseases (ICD) Over the years, diseases have been classified in a number of ways, e.g. diseases of the chest, or diseases caused by bacteria, but in 1893, the first edition of an international diagnostic classification system called the International Classification of Disease (ICD) was adopted. Since then it has been refined nine times to the point when the current version, ICD-10, came into use in 1994. On page 22 of Gilles and Lucas (2003), you will find box 2.5 which provides the broad classifications. This system is used by the WHO member states for many types of health and other vital records, including death certificates; they are used for a variety of purposes including compiling national mortality and morbidity statistics for the purpose of measuring health and disease. The use of standard classification of diseases and injuries has greatly aided the statistical analysis of morbidity and mortality data. Through the United Nationals and the World Health Organization, an internationally recommended classification has been evolved, which is periodically revised. Although this SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 72 classification may be extended or modified to suit local and national conditions, the essential structure for international comparisons must be preserved. Lucas and Gilles, 2003: 21) These diagnostic codes have also gained an important role in Public Health practice. For example, if you are required to measure and manage the spread of diseases, you certainly need some system to cluster disease types. An important application of the ICD system has been the development of a tool for measuring ill health as well as mortality for the purpose of health system planning. The WHO website provides a link to the current version and a history of the development of the ICD (WHO, 2009). TASK 6 – Familiarise yourself with the ICD system To familiarize yourself with the ICD, log on to the following website: http://www.who.int/classifications/icd/en/. This takes you to the International Classification of Diseases (ICD) homepage. Follow these steps and questions. Under ICD-10 ONLINE click on “Current version”: 1. Scan though site and describe how the classification is organised. 2. Find the ICD codes for the following diseases: tuberculosis helminthiases HIV/AIDS 3. How easy or difficult did you find this process? 4. Identify three ways in which ICD is used in your country. If you do not find any, can you think of three ways in which it could be used in your country? How would this be helpful? FEEDBACK 1. Did you notice that the ICD system it is fairly clinical and complex but is organised by groups of causes in some clusters, per organ in others, per life stage in others? 2. You will find that by simply typing “tuberculosis” and “full search” in the search field located in the left column, your reply is that there are too many results (over 200). Limit your search to “titles only” by pre-selecting it from the drop-down menu. This will give you a whole page of codes and sub-codes for tuberculosis. Notice that ICD-10 is very specific about different types of TB with A15 being, for example, Respiratory TB, bacteriologically or histologically confirmed. Besides this, there are a number of other TB conditions listed in ICD 10. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 73 3. Your own reflection. If you found this difficult, what could you do to make the process easier in future? 4. You may have found that the codes are used to classify disease and health problems recorded on death certificates and health records. Those of you from South Africa may remember the introduction of compulsory ICD codes on clinical diagnoses for medical insurance purposes. 4.2 Organising diseases into four broad groups The ICD-10 classification is very specific as you will have noticed. For the purpose of the Global Burden of Disease (GBS) study, health conditions were further combined into three broad groups which would provide a global picture of disease burden which would be relevant for health policy and planning (Lopez et al, 2006). These groups have become incorporated into Public Health discourse to the extent that countries are said to suffer under a double or triple burden of disease, depending on which groups dominate. Arising from the increasing burden of HIV/AIDS in subSaharan Africa, some literature has separated it from Group I and created a fourth category, referred to as a quadruple burden of disease. Group I Communicable diseases, maternal, peri-natal and nutritional conditions. See Group IV. Group II Non-communicable diseases Group III Injuries Group IV Due to the increasing burden of HIV/AIDS, some countries have separated it from the rest of Group I as a fourth category, as is the case in South Africa. TASK 7 – Classify health conditions in the main disease groups Classify the following conditions by Group: 1. 2. 3. 4. 5. 6. 7. Malaria Injuries from road traffic accidents Heart attack Bi-polar depression Diabetes Severe malnutrition TB SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 74 FEEDBACK These conditions should have been classified as follows: 1. 2. 3. 4. 5. 6. 7. Malaria – Group I Injuries from road traffic accidents – Group III Heart attack – Group II Bi-polar depression – Group II Diabetes – Group II Severe malnutrition – Group I TB – Group I This concludes the introduction to the main concepts and terminology needed at this stage. You will revise it as you work through the modules. By now, many of these terms are hopefully beginning to be familiar to you, or you should at least know where to look in order to clarify unfamiliar concepts. In the final section of this Study Session, we explore some of the sources of health information with which we would like you to become familiar. 5 SOURCES OF INFORMATION FOR HEALTH In order to undertake measurement of populations, the essential ingredient is reliable data. You therefore need to be in a position to locate it and access it. This is the purpose of this section: the extent to which you will learn from this section depends on the effort you put into finding local and international sources of information. Start off by reading page 12 of your setwork for an orientation to the kinds of information which is used in the field of Public Health; in addition, explore this section for sources of health statistics. READING Lucas, A. O. & Gilles, H. M. (2003). Ch 2 – Health Statistics: Information for Health. Short Textbook of Public Health Medicine For the Tropics. 4th ed. London: Arnold Publishers: 11–14. A picture of the health of a population may be derived by accessing and analyzing data from a variety of sources. The types of information you need to know about is: Your population - its size and age/sex distribution as well as geographical distribution and socio-economic status. Disease burden - causes of mortality (what people are dying of) and morbidity (what diseases people are living with). Risk factors (underlying causes of the diseases). This information is important for health systems planning, management and evaluation, at a local, national or global level. Read these pages of a chapter on health data, in particular page 195 before tackling Task 8. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 75 READING Birn, A-E., Pillay, Y. & Holtz, T. H. (2009). Ch 5 – What Do We Know, What Do We Need to Know, and Why it Matters – Data on Health. Textbook of International Health: Global Health in a Dynamic World. New York/Oxford: OUP: 192–224. TASK 8 – What routine data is collected in your country? 1. Find out by searching the internet or making enquiries in local institutions or amongst your colleagues what kinds of data are collected and made available to the public in your country. Search for sources at a local (district) and national level and say what type of information they provide. 2. Develop a word table listing this data which looks something like this: Sources of routine health data in South Africa Name of database and source organisation Source Type of data organisation How to access it Regularity of update FEEDBACK 1. In South Africa, we have relatively good publicly available sources of information on the internet. These sites include: You should explore these South African sites or look for comparable sites in your own country: Organisation The Human Sciences Research Council The Population Council of South Africa The National Injury Mortality Surveillance System (NIMSS) in The Medical Research Council Website address http://www.hsrc.ac.za/ South Africa – Department of Health http://www.doh.gov.za/ http://www.popcouncil.org/africa/southafrica.html/ http://www.mrc.ac.za/ There are probably other sites, particularly at local level. Remember that anyone can put information onto the Internet. So take care to check that the websites you use are reliable, and that data accuracy is prioritised by the provider. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 76 Finally, it is important that you keep building up your own resource of addresses for these types of Internet sites and that you become familiar with what they contain, but also, that you are aware of their limitations. Try to build this information by searching the Internet, by speaking to experienced colleagues, and by talking to others involved in epidemiology in your country. 2. Here is an example of the kind of information you might collect. Sources of routine health data in South Africa Name of database and source organisation Source organisation Type of data How to access it Regularity of update Population census: Labour Force Surveys; October Household Surveys; Mortality Reports. Statistics South Africa (who undertake the census) Population data; vital statistics; employment [Online], Available: http://www.statss a.gov.za/ 5 years 6 SESSION SUMMARY In this session, you have been guided through the meaning of a range of key concepts in Public Health measurement and orientated to locating sources of reliable health data in your country and on the Internet. You have also been introduced to the classification system for diseases, the ICD-10 codes, and the broad groups of disease into which diseases have been organised for the purpose of understanding the global burden of disease. In the next session, the Global Burden of Disease studies will be introduced in more detail, as will the Health Transition or trend from communicable disease to noncommunicable disease which has been witnessed in developed countries, and is being monitored in developing countries. Take a well deserved break before proceeding to the next session. 7 REFERENCES AND FURTHER READING Beaglehole, R. & Bonita, R. (2001). Public Health at the Crossroads: Achievements and Prospects. Auckland, New Zealand: Cambridge University Press. Centres for Disease Control (n.d.) Lesson 2: Frequency Measures Used in Epidemiology. [Online], Available: http://www2a.cdc.gov/phtn/catalog/pdffile/LESSON2.pdf. [Downloaded: 17.1.10]. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 77 Joubert, G. & Ehrlich, R. (eds). (2007). Epidemiology: A Research Manual for South Africa. Cape Town: Oxford University Press. Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T. & Murray, C. J. L. (2006). Global Burden of Disease and Risk Factors. Washington & New York: World Bank and Oxford University Press. Miller, J. A., Baehr, G. & Corwin, E. H. L. (1942). Preventive Medicine in Modern Practice. New York, NY: PB Hoeber Inc. The Namibian. (Windhoek) [Online] Available: http://www.namibian.com.na/ [Downloaded 25 November 2009]. UNICEF (United Nations Children’s Fund) and the World Health Organization. (2004). Low Birth Weight: Country, Regional and Global Estimates. New York: UNICEF. Vaughan, J. P. & Morrow, R. H. (1989). Manual of Epidemiology for District Health Management. Geneva: WHO. Walley, J., Wright, J. & Hubley, J. (2001). Public Health: An Action Guide to Improving Health in Developing Countries. Oxford: Oxford University Press. WHO (1948). Constitution of the World Health Organization. Geneva: World Health Organization. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 78 Unit 2 – Study Session 2 Populations and Health Introduction In the previous session we introduced you to some of the common measures used to describe health and disease in populations. In this session you will learn a little more about ways in which populations are described in terms of their size and composition and how they change over time and the factors that influence those changes. We will also look at the distribution of diseases and their risk factors in populations and introduce you to the concept of the Burden of Disease. Finally we will look at the value of burden of disease data in planning health services, and monitoring and improving the health of populations. Contents 1 2 3 4 5 6 7 8 Learning outcomes for this session Readings Demography and population pyramids The health transition – demographic and epidemiologic transitions Global burden of disease studies Comparative Risk Assessment (CRA) Session summary References and further reading SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 79 1 LEARNING OUTCOMES OF THIS SESSION By the end of this session, you should be able to: Health measurement outcomes Academic learning outcomes 2 Demonstrate familiarity with the concept of demography. Discuss the Health Transition. Demonstrate an understanding and describe the value of Burden of Disease studies. Describe the concept of comparative risk factor assessment. Explain challenges in compiling Burden of Disease and comparative risk assessment data. Understand a range of graphs including population pyramids Compare information to assess its relative value or the risk factors present Develop critical listening skills Identify and extract relevant information from a range of data and texts Apply advanced reading skills of skimming and scanning for critical information READINGS The readings for this session are listed below. You will be directed to them in the course of the session. Author/s Beaglehole, R. & Bonita, R. Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T. & Murray, C. J. L. Bradshaw, D. Norman, R., Bradshaw, D., Schneider, M., Joubert, J., Groenewald, P, Lewin, S., Steyn, K., Vos, T., Loubscher, R., Nannan, N., Nojilana, B. & Pieterse, D. (South African Comparative Risk Assessment Collaborating Group) Publication Details (2001). Ch 1 – Health, disease & the health transition. Public Health at the Crossroads: Achievements and Prospects. Auckland, New Zealand: Cambridge University Press: 6–11. (2006). Global and Regional Burden of Disease and Risk Factors, 2001: Systematic Analysis of Population Health Data. Lancet, 367: 1747–1757. Interview with Prof Debbie Bradshaw of the Medical Research Council of South Africa on the Burden of Disease study in South Africa. (see CD). (2007). A Comparative Risk Assessment for South Africa in 2000: Towards Promoting Health and Preventing Disease. South African Medical Journal, 97: 637–641. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 80 3 DEMOGRAPHY AND POPULATION PYRAMIDS 3.1 Describe populations The study of populations or demography is described as the scientific description of “… the size and characteristics of the population, including age and sex, spread across geographical areas and changes over time” (Bourne & Joubert, in Joubert, Ehrlich with Katzenellenbogen, 2008: 24). Demography embraces all aspects of population structure and changes which can be measured numerically. This includes primarily: measurement of the size of the population (how many people there are); composition (the characteristics of people such as age and sex); distribution (where the people in the region are); changes in numbers of people. The main demographic processes which lead to changes in the number of people and composition of a population are fertility, mortality and migration. So, having an accurate estimate of the population size is the first pre-requisite. Drawing on the above definition we can describe the composition or characteristics of a population using a number of parameters, including: Age Gender Occupation Income “Race” or ethnicity Education TASK 1- Link demography and Public Health 1. Now think for a moment – what value does demography have for Public Health? FEEDBACK 1. The way in which a population is distributed geographically throughout a country or a district is important, especially in planning and delivering health services. How the population size changes over time is also a key consideration in health services planning and delivery. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 81 Returning to the definition of demography again, we see that population size is affected by three factors namely: FERTILITY MORTALITY MIGRATION (BIRTHS) (DEATHS) (IN-AND OUT-MIGRATION) So having accurate information on these factors is essential in order to compile a reliable population profile. The relationship between these three factors determines whether the population size increases, decreases or remains stable. 3.2 Population pyramids Population pyramids are diagrammatic or visual ways used to illustrate the population composition according to age and sex distribution. Some literature, like your Vaughan & Morrow (1998) terms them graphical representations. They are based on population census data. Their purpose in relation to health is to provide estimates of the “at-risk population” to calculate “certain age- and sex-specific rates” (Vaughan & Morrow, 1998: 23). Look at the three diagrams below which are population pyramids for three countries: Fig 1 - A Lower Income or developing country, e.g. Kenya in 2008 Fig 2 - A middle-income or transitional country, e.g. South Africa in 2008 and Fig 3 - A developed or Higher Income country, e.g. France in 2008. These three population pyramids come from the website of the United States Census Bureau. You can go onto the site and see whether your own country’s data is provided for any particular year. The site also provides demographic indicators which may be of interest. You can select the country and the year, select several years to compare them and you can also gather demographic data as well as population tables. Please note that some queries, e.g. Zambia 2008 do not have data. The site is at: http://www.census.gov/ipc/www/idb/country.php SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 82 Fig 1 - A Lower Income or developing country, e.g. Kenya in 2008 Fig 2 - A middle-income or transitional country, e.g. South Africa in 2008 SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 83 Fig 3 - A developed or Higher Income country, e.g. France in 2008 Read the population pyramids The population is represented by horizontal bars. You will see that the y-axis represents age, and is divided into 5-year age groups, with the youngest at the base. The x-axis has the population in thousands. Some diagrams may indicate the percentage of population on the x-axis The usual convention is that population pyramids have males on the left side of the graph and females on the right. TASK 2- Interpret a population pyramid 1. You will notice that the shape of the population pyramids of these three countries are different. What does this tell us FEEDBACK 1. These differences in shape are the result of variations in births, deaths and migration in each of the populations. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 84 The table below draws out key points regarding the population pyramids in the figures and indicates what we can learn about these populations. Table 1 - Compare three population pyramids Characteristics Figure 1 SHAPE Trianglular BASE Broad – high birth rate DESCRIPTION Tapers off quickly – low life expectancy High proportion of population is young and not many older people TYPICAL OF Developing country HEIGHT Figure 2 Boat shaped Broad – high birth rate but widens at age 15-20 then narrows Tapers off more gradually than Kenya High proportion of 15 – 20 year olds; more older people than in Fig 1 but tapers more steeply than in Fig 3. Middle income/transitional country Figure 3 Onion-shaped Narrow – lower birth rate Steep sides – higher life expectancy Proportion of children in population is smaller and there are larger numbers of middleaged and elderly Developed country The shape of Figure 1 is a step pyramid or triangle with a broad base and tapers off quickly. In this population, a large proportion of the population is young, but there are not many older people. We can deduce that this population has a high birthrate and a low life expectancy and is typical of a developing country. Figure 3 looks more like an onion in shape. The base of the graph is smaller than some of the other bars and the pyramid is at its widest at 35-55 years of age; it tapers off gradually. This shape is typical of developed countries where the portion of children in the population is smaller than developing countries where there are large numbers of middle-aged and older people in the population. This population typically has a low birthrate and high life expectancy. Figure 2 falls somewhere between Figures 1 and 3 and is typical of a middle-income country that is partly industrialized, but not as developed as the economy in Figure 3. Note that the unusual shape of Figure 2 is most likely the result of HIV/AIDS in South Africa which has given rise to increased infant mortality over the past few years. It is hoped that the situation will change soon, as antiretroviral treatment for mothers and infants becomes widespread: this would decrease the numbers of babies born with HIV and in this way decrease the numbers of infants and children dying of HIV. TASK 3 – Familiarise yourself with demographic data 1. Log on to the above website and look at the population pyramids for a range of countries around the world; note the differences, and compare them with above examples. Make sure you take a look at Sweden in 2008, as it is very different from these three. What does it tell you about the health of Sweden’s population? 2. Now use the website to look at the most recent population pyramid for your own country and use it to describe the population. Use the table above to guide you. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 85 3. Which of the three figures above does your country population pyramid most closely resemble? 4. How do you think the population pyramid of your country could assist you in planning health services? FEEDBACK 1. 2. 3. 4. 4 No feedback will be provided. No feedback will be provided. No feedback will be provided. The population pyramid enables you to identify the largest proportions of the population as well as the age groups which require services. For example, if a high proportion of the population is under-5 then the country would need to prioritize maternal and child health services. On the other hand, if there are a large numbers of older people, then services for the elderly and for chronic disease prevention and management would be important. These might include provision of medicines for chronic conditions and rehabilitation services. In this way, demographic data becomes key information for Public Health policy and planning. THE HEALTH TRANSITION - DEMOGRAPHIC AND EPIDEMIOLOGICAL TRANSITIONS As we have already mentioned, populations change over time and along with these changes there have been significant changes in the patterns of health and diseases. Over the past few decades there has been a transition in the type and distribution of illness in the global population which has come to be known as the Health Transition. Shifts from, for example, the prevalence of primarily communicable diseases to noncommunicable diseases is currently regarded as the Health Transition. Higher income countries that once experienced epidemics of plague, flu and other infectious diseases now contend with increased health problems from noncommunicable diseases like cancer, hypertension and diabetes affecting their large older population. In higher income countries, the impact of communicable diseases commonly associated with poverty has been gradually reduced with extensive immunisation programmes contributing to these gains. These hard won achievements have, however, been dramatically reversed by HIV/AIDS. On the other hand, lower income countries, e.g. Kenya and middle income (such as South Africa) continue to carry the burden of many of the communicable diseases plus HIV/AIDS, with a rising tide of non-communicable diseases. Beaglehole & Bonita (2001: 6) describe the Health Transition as … a framework for describing and explaining the spectacular shifts in the patterns and causes of death that have taken place in most countries”. It is a conceptual model that was developed SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 86 in the early 1990s building on the prior ideas of the Demographic Transition and the more recent idea of the Epidemiological Transition. Beaglehole and Bonita (2001) citing Feachem, Kjellstrom, Murray, Over & Phillips (1991), explain: Demographers originally used the term ‘demographic transition’ or ‘mortality transition’ to describe the change from high fertility and mortality rates in ‘traditional’ societies to low fertility and mortality rates in ‘modern’ societies. [Citing Omran, (1971)] they note that [a] broader term, ‘the epidemiological transition’, was introduced to describe, in addition to mortality, the long-term changes in patterns of sickness and disability that occurred as societies change their demographic, economic and social structure. (Beaglehole & Bonita, 2001: 6) The Health Transition is a very complex process affected by a range of social, political, economic and environmental factors as well as technical developments and growing knowledge of diseases and their causes. In addition, because of the way our lives in the “global village” are now connected through communication, transport and economic forces, the health of remote communities can be affected by global in addition to local determinants. For example, think of the arrival of fast foods in developing countries, and how it disrupts nutrition patterns and therefore the health of populations. Public Health workers need to recognise the influence of these factors as they struggle to improve the health of communities. Start with Task 4 to see whether you see evidence of the Health Transition in a set of population pyramids. TASK 4 – Look for evidence of the Health Transition Log on to the US Census Bureau website again at: http://www.census.gov/ipc/www/idb/country.php 1. Look at population pyramids over time (e.g. 1979, 1992, 2008) and note if they are the same or different for a: Developed country You may have to search for dates when there is Developing country census data, e.g. there Your own country. 2. Now look at the population pyramids for South Africa in 1985, 1992, 2008 and note if they are similar or different. If different, why do you think they are? is nothing for Zambia in 2008. Note that you can load a number of population pyramids at the same time and flip between them using the animation controls. Hold down Ctrl on your keyboard and select the years you would like to view SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 87 FEEDBACK 1. The population pyramids for South Africa have changed significantly over the past 20 years. South Africa is described as a transitional country, that is, somewhere between a developed and developing country. In fact it has a highly unequal distribution of income and wealth because of almost 50 years of apartheid policy. 2. It has also experienced considerable changes over the past few years. Reductions in fertility and child mortality, and increases in life expectancy are reflected in the changes in the demographics of the SA population as shown in the population pyramids and so it has been concluded by researchers in South Africa that the population is experiencing a demographic transition and at the same time, a Health Transition. Read the extract by Beaglehole & Bonita and try Task 5 at the same time. READING Beaglehole, R. & Bonita, R. (2001). Ch 1 – Health, disease & the health transition. Public Health at the Crossroads: Achievements and Prospects. Auckland, New Zealand: Cambridge University Press: 6–11. TASK 5 – Use these questions to clarify these concepts The authors are critical of the concept Demographic Transition which was used previously because: … [complete the sentence]. 1. What is the link between Health Transition and mortality rates? 2. What is the main pattern they identify in Health Transitional societies? 3. What is encompassed by the fourth phase of the Health Transition? 6. Why do the authors favour the concept, Health Transition over Epidemiological Transition? 7. What do they say are the main factors which propel the Health Transition? 8. Write a short description of each. Do you think this covers all factors? 9. What critical points do they raise regarding the notion of the Health Transition? SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 88 FEEDBACK Here is selected feedback for you to check your understanding against, but the answers are in the text. 1. The link between Health Transition and mortality rates is that the model has been developed to explain changes in mortality rates as well as birth and fertility rates over time. 2. The authors identify a number of deficiencies in the Health Transition model: It has little ability to predict changes associated with modernization. It does not explain mortality differences between countries. It is sometimes seen outside of the socio-economic factors which propelled it. A number of country-based anomalies exist which cannot be explained by it. And … in its original form – the Epidemiological Transition: focused on the shift from communicable to non-communicable diseases, and did not consider deaths from injuries. does not take account of declines in mortality in some non-communicable diseases and is of limited predictive value. Before we conclude, here is a little more background information about the Demographic Transition. 4.1 Demographic Transition Although this term is viewed critically in relation to developing country contexts by Beaglehole and Bonita (2001), it is necessary to understand the concept Demographic Transition, also known as the Mortality Transition. The concept refers to a model used by demographers to explain changes in the birth, fertility and death rates in industrialized populations over the past two hundred years. The basis of this model arose in the work of the American demographer Warren Thompson in 1929, and was based on observed changes in birth and death rates in industrialized societies over approximately the past two hundred years. By "model" we mean that it is an idealized, composite picture of population change in these countries. The model is a generalization that applies to these countries as a group and may not accurately describe all individual cases. Whether or not it applies to less developed societies today remains to be seen. Montgomery, K. The Demographic Transition. Dept of Geography and Geology. [Online], Available://http: www.uwmc.uwc.edu/geography/Demotrans/demtran.htm The Demographic Transition is divided into four stages coinciding with the urbanization and industrialization of societies: Stage one: Stage two: Pre-modern societies Urbanising/industrialising SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 89 Stage three: Stage four: Mature industrial Post industrial Here is the here is the model taken from the website cited in the box above (Montgomery, n.d.). You can read more about the model by following the link provided in the box above. (Source: Montgomery, K. The Demographic Transition. Dept of Geography and Geology.) More recently (1971), a model of Epidemiological Transition was advanced by Omran. 4.2 The Epidemiological Transition The concept Epidemiological Transition describes the long term changes in patterns of mortality, morbidity and disability that have arisen from changes in the demographic, economic and social conditions of populations (Beaglehole & Bonita, 2001). These changes correspond with the stages of demographic transition. Omran (1971) proposed three stages of the Epidemiologic Transition: SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 90 1 Age of pestilence and famine. 2 Age of receding pandemics. 3 Age of degenerative diseases, now called non-communicable disease or chronic diseases. The first stage, “the age of pestilence” was characterized by mortality due to communicable diseases and poor maternal and child health; life expectancy was generally low. In western countries, the second stage spanned the 18th and 19th centuries and was characterized by infectious diseases and malnutrition, but with a higher life expectancy than the previous stage. The third stage is dominated by non-communicable diseases and characterized by lower fertility rates and higher life expectancy. Omran (1971) described how, as diseases associated with underdevelopment decline, e.g. communicable diseases and poor maternal and child health, most societies show a concomitant increase in non-communicable (chronic) diseases associated with unhealthy patterns of living. These changes are mainly attributable to the following risk factors: increasing urbanization; changes in dietary consumption (increase in foods high in animal fat, salt and sugar); decreased physical activity; iincreases in smoking and alcohol use. Olshansky and Ault (1986) proposed a fourth stage to the Epidemiological Transition: 4 Age of delayed degenerative diseases. In conclusion, we need to be aware that the Health Transition (the preferred concept) in poor countries may not necessarily follow the same pattern as has occurred in the western industrialized countries. A number of authors Including Beaglehole & Bonita (2001) have cited variations on the models in the developing world context. Furthermore, they raise the problem of In South Africa, we also suffer a considerable burden of intentional and non-intentional injuries (Group III causes of mortality and morbidity), as well as the HIV/AIDS epidemic which has been allocated a separate disease group category (as you learnt in Unit 2 Session 1). Consequently, South Africa may be experiencing a Health Transition, but may be said to be suffering a quadruple burden of disease. In spite of the limitations of the model, the Health Transition remains a useful framework for describing changes in mortality and disease patterns. So far in this session we have looked at how populations are described in terms of demography and at changes in populations over time - due to demographic factors SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 91 such as births, deaths and migration, as well differences between different populations. We have also looked at other factors that affect disease patterns. In the next part of this session we will look more closely at a type of study (the Global Burden of Disease study) which provided evidence of the Health Transition within global profiles. Here is an extract: In the first GBD study, non-communicable diseases, including neurological and psychiatric ailments, were estimated at 41% of the global burden of disease in 1990, with 44% due to communicable, maternal, perinatal and nutritional conditions combined, and 15% due to injuries (Murray and Lopez, 1996). Fifty-five percent of all deaths worldwide were found to be due to non-communicable diseases; 35% to communicable diseases; and 10% to injuries. An updated GBD study found that in 2001 58.5% of all deaths and 52.6% of the global burden of disease worldwide were due to noncommunicable diseases; 32.3% of all deaths and 36.5% of the global burden of disease were due to communicable diseases, perinatal conditions, and nutritional deficiencies; and injuries accounted for 9.2% of all deaths and 10.9% of the global burden of disease (Lopez et al, 2006a). As in 1990, approximately one third of deaths were in Group I (virtually all in low-and middle-income countries); however HIV/AIDS went from 2% of Group I deaths in 1990 to 14% in 2001. Altogether, the three leading causes of death in 2001 were ischemic heart disease, cerebrovascular disease, and lower respiratory infections. These diseases together accounted for almost 20% of all deaths in low- and middle-income countries, … demonstrating that there is a simultaneous burden of infectious and non-communicable diseases (Lopez, 2006a). The 2004 update of the GBD showed that the three leading causes of death had increased to comprise 29% of all deaths in low- and middle-income countries (WHO, 2008). (Birn, Pillay & Holtz, 2009: 228). Note how the global burden of disease is reported: deaths are estimated worldwide for a particular year as percentages (underlined) attributed to particular disease groups. This is followed by the percentage of the global burden of disease attributed to each particular disease group (see bold text above). 5 GLOBAL BURDEN OF DISEASE STUDIES A burden of disease study is a particular type of study that aims to estimate the overall burden of disease and its causes. This requires substantial amounts of data, including cause of death statistics, incidence of conditions and the duration and severity of the diseases or disability. Most countries, SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 92 including South Africa, do not have all the requisite data for such a study. However, they do have several sets that can be used together with mathematical models of disease dynamics and population demographics to derive reliable estimates of the burden of disease. An essential component of such a study is a critical analysis of the available data to investigate the agreement between them so as to derive consistent and coherent estimates of the burden of disease. (Bradshaw, in Joubert & Ehrlich, 2008: 200-201). 5.1 Background The original Global Burden of Disease (GBD) Study was commissioned in 1991 by the World Bank to provide a comprehensive assessment of the 1990 global disease burden for 107 diseases and injuries and ten selected risk factors in eight geographical regions of the world. Christopher J. L. Murray and Alan D. Lopez (working at the WHO) devised the tool for measuring the relative burden of disease carried by different countries. Previous work had focused on quantifying global cause of death (mortality); a key feature of the GBD framework was the incorporation of non-fatal health outcomes to provide an overall measure of population health. The GBD study “used a common metric [or established measurement] to summarize the disease burden from diagnostic categories of the International Classification of Diseases (ICD) and the major risk factors that cause those health outcomes” (Lopez, Mathers et al, 2006:1). The GBD study is elaborated by Friis and Sellers (2004) as follows: The GBD attempts to quantify and provide an epidemiologic assessment of the worldwide consequences of disease by using a measure known as the disability-adjusted life year (DALY) to assist in comparison across countries. The DALY is a statistical measure applied to populations that combines information on mortality with information on morbidity for specific causes. The advantage of DALYs is that they provide a standard epidemiologic unit for comparative purposes. 5.2 DALYS (disability-adjusted life years) The “disability-adjusted-life-year” or DALY was the metric devised for the GBD study (Walley, Wright & Hubley, 2001: 6). DALYs comprise Years of Life Lost or YLLs due to premature death AND YLDs (Years Lived with Disability) weighted according to the severity of the disability. The sum of the two components, namely, DALYs, (disability-adjusted life years) provides a summary measure of the future stream of health life (years expected to be lived in full health) lost as a result of disease. DALYs highlight the burden caused by diseases that cause disability (non-fatal outcomes), rather than exclusively mortality (deaths). This includes mental and nervous disorders. 1 DALY = 1 year of healthy life lost SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 93 The sum of the two components, YLL and YLD makes up DALYs, (disability-adjusted life years) and provides a measure of the future stream of health life (years expected to be lived in full health) lost as a result of disease. YLLs (Years of Life Lost) as a result of premature death when compared to a full lifespan; the measure takes into account age, emphasizing premature mortality and providing an important indication of diseases resulting in many early deaths. So, diseases that occur mainly in older people such as cardiovascular disease contribute less to the YLL burden than homicide and violence which are more common in younger people. YLDs (Years Lived with Disability) weighted according to the severity of the disability Morbidity on the other hand was measured in terms of days of illness, ranging from several days in the case of acute illnesses, e.g. measles, to years of disability with, for example, deafness. The proportion of morbidity and mortality varies from disease to disease. More DALYs are lost from disability in the case of depression and leprosy. In contrast, a disease with a high mortality, such as tuberculosis, will result in more DALYs lost through premature death. (Walley, Wright & Hubley, 2001: 6). Remember that the disease classifications underpinning these measures are the diagnostic categories from the ICD and the overarching four categories of disease (e.g. Group I - Communicable maternal, peri-natal and nutritional conditions). 5.3 What do Burden of Disease (BOD) studies tell us? What have we learned from the GBD studies? What have we gained? The GBD provides an understanding of the relative burden or consequences of disease within and across countries and regions. In addition, the successive GBD studies (original study was completed 1991, superseded in 2001 by a revised study, and updated in 2004) have provided the opportunity to track trends over time. A new round of the GBD study using 2005 data is under way and will be published at the end of 2010, mapping trends from 1990 to 2005. This Foreword by Samuel H. Preston to Global Burden of Disease and Risk Factors (2006) captures some of the achievement of the study. 'Every observer of human misery among the poor reports that disease plays the leading role.” Irving Fisher (1909, 124) Before 1990, the global disease landscape was perceived “through a glass darkly.” Mortality conditions by cause of death were known with some SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 94 precision only for the relatively small minority of the world’s population residing in countries with adequate vital statistics. Nowhere were estimates of disease incidence, prevalence, survival, and disabling sequelae consistently combined into population-level profiles of morbidity and mortality. Publication of the Global Burden of Disease (1990) was a watershed event in the assessment of health and disease. Through careful synthesis of disease conditions revealed in thousands of piecemeal studies and data systems, it constructed a comprehensive portrait of diseases, injuries, and causes of death. It dealt creatively and carefully with the hundreds of issues that had to be addressed to develop useful, broadly gauged indicators of health. These included establishing terms of trade among disabling conditions, among age groups and generations, and between the living and the dead. At all points that offered tempting shortcuts, the authors decided in favor of comprehensiveness. Like the microscope, the Global Burden of Disease (1990) brought diseases into much sharper focus. Like national income accounts, it connected parts to a whole and measured the whole with unprecedented precision. As a sophisticated measuring device, it could not be ignored by any serious student of epidemiology or development. One might have experimented with its calibrations, but the device itself was irreplaceable. However, the value of a measuring device lies in its measurements, not in its abstract qualities on the shelf. The world has changed dramatically since 1990, and we must be grateful for the fresh assessment of disease conditions presented in this volume. The picture that it paints is not only updated; it is also more precise. Better data have become available through expanded vital statistics systems, improved surveys, and more extensive population surveillance systems. The measurement instrument has also been improved. Most notably, a critical new layer of physical risk factors and their distribution has been added, providing valuable new tools for policy makers. This second application of the global burden of disease framework permits an analysis of trends observed since the first application. The intervening period was clearly one of slow progress, impeded by the HIV/AIDS epidemic and setbacks in Eastern Europe. The volume is appropriately cautious in drawing inferences about disease-specific trends because of changes in data sources and, in some instances, improvements in approaches to measurement. The volume also contains a valuable and admirably frank chapter on the sensitivity of estimates to various sources of uncertainty in methods and data. Some estimates are found to have wide bands of uncertainty. While this outcome is disappointing, uncertainty about the burden of disease in all its dimensions—including the degree of uncertainty itself— would be much greater without the heroic efforts reflected in this volume. My congratulations to the authors and the sponsoring agencies. Samuel H. Preston, Fredrick J. Warren Professor of Demography, University of Pennsylvania SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 95 Irving Fisher. 1909. Report on National Vitality, Its Wastes and Conservation. Prepared for the National Conservation Commission. Washington, DC: Government Printing Office. The GBD study confirmed what many health workers had suspected - that noncommunicable diseases and injuries were a significant cause of health burden in all regions of the world, including developing countries. Furthermore, it was through the capacity of the GBD to measure morbidity in addition to mortality, that the effect of neuro-psychiatric diseases and injuries were appreciated. TASK 6- Familiarise yourself with the GBD website 1. Now explore this website to see what sort of information the burden of disease study provides: WHO. Burden of Disease Statistics. [Online], Available: http://www.who.int/healthinfo/bod/en/. [25 2 07]. FEEDBACK 1. In order to understand better what the 2001 GBD study tells us about the burden of disease and the risk factors which fuel the burden, read the article below. READING Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T. & Murray, C. J. L. (2006). Global and Regional Burden of Disease and Risk Factors, 2001: Systematic Analysis of Population Health Data. Lancet, 367: 1747-1757. This article reports on the global and regional burden of disease and risk factors in 2001, presenting results for the World Bank’s designated regions. High-income countries are shown as one group and low and middle income groups are divided into six geographical regions. You will note that the authors spend some time explaining the methodologies that were used and you will see that it is a very complex process: we do not expect you to grasp all the details. However, it is important to remember that the estimates of mortality and disease burden are calculated using data from a variety of sources; where the information is not available, statistical modeling is used to develop estimates. The authors note that information from sub-Saharan Africa was particularly lacking. Read the paragraph titled “Findings” in the “Summary” or abstract at the beginning of the paper again, to refresh your understanding of the overall results of the GBD study and study Figures 1 and 2 and Table 1. Figures 1 and 2 on pages 1749 and 1748 in the reading show death rates by disease group and region in 1990 and 2001 for children aged 0-4 years and adults aged 15-49 years respectively. The first thing that will strike you is that death rates in sub-Saharan SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 96 Africa region are the highest for both children aged 0-4 years and adults. You will also notice that between 1990 and 2001, child mortality fell in all regions and that adult mortality fell in all regions except Europe and Central Asia region and sub-Saharan Africa region. Look again Figure 1 and identify what proportion of the deaths in the sub-Saharan Africa region are attributed to conditions in Group 1, that is malaria, diarrhoeal disease, respiratory infections, other infections and parasitic disease, perinatal cases and nutritional deficiencies. Look now at Figure 2 and note which are the most common causes of death in sub-Saharan Africa and how the situation has changed between 1990 and 2001. The table below is summarized from Table 1 in the reading and shows the top 10 causes of death by income group. Ischaemic heart disease and cerebrovascular disease were the leading cause of death in both income groups. In the low income group, five of the top ten causes are infectious disease; that is lower respiratory infections, HIV/AIDS, diarrhoeal diseases, tuberculosis and malaria. Complete the table from the article. Ten Leading Causes of Death by Income Group, 2001 Low and middle income group Cause 1 2 3 Ischaemic heart disease Cerebrovascular disease Lower respiratory infections Deaths (millions) % of total deaths 5.70 11.8% 4.61 9.5% 3.41 7.0% High income countries Cause Ischaemic heart disease Cerebrovascular disease Deaths (million s) % of total deaths 1.36 17.3% 0.78 9.9% 4 5 6 7 8 9 10 (Source: Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T. & Murray, C. J. L. (2006). Global and Regional Burden of Disease and Risk Factors, 2001: Systematic Analysis of Population Health Data. Lancet, 367: 1747-1757.) You will remember that the second part of the GBD study studied premature death and disability; Table 3 in the reading shows the 10 leading causes of the Burden of Disease (DALYS) by income group. The authors say that the global picture was broadly similar to the low and middle income group and included five communicable diseases. The leading causes in high income groups were all non-communicable diseases (Group II causes). You will note that the ranking of diseases changes between deaths and Burden of Disease. Look back at the note in 5.2 to remind yourself why this happens. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 97 The third part of the study was to measure the mortality and burden of disease in relation to leading global risk factors. It was found that an estimated 45% of global mortality and 36% of the global disease burden were attributable to the 19 selected risk factors. The results are shown in Figure 5 and again you will notice the difference in ranking between mortality and burden (DALYS). The authors conclude by stressing the need for the type of data produced by the GBD study to monitor population health and the effects of specific policies. They acknowledge the methodological challenges of their work but conclude by saying that work in improving the data is ongoing. The updated GBD study can be found on the WHO website and may be downloaded free of charge. http://www.who.int/healthinfo/global_burden_disease/2004_report_update If you click on the web address below you can find more information on the GBD 2004 update under “Multimedia” http://www.who.int/healthinfo/global_burden_disease/en/ TASK 7 - Extract BOD data from the WHO website 1. Try to find BOD information for the two countries you selected earlier. List the top 10 causes of death in each country for males, females and the whole population in the following three ways: based on number of deaths based on death rates using DALYs 2. Compare the ranking of the different causes of death and explain the reasons for the differences and how the various measures contribute to providing a picture of the burden of disease in these countries. 3. What contributions do DALYs make to understanding the burden of disease in these countries? FEEDBACK 1. On the provided URL, under “Statistics” choose “disease and injury – country” in order to get information on deaths and DALYs. This opens up “Disease and injury estimates”. You should then choose the appropriate MS Excel file for each of the persons, males and females. Your selected country should now appear from which you can select the top 10 conditions. 2. Depending on the two countries you have chosen, you should have found some important similarities and differences in rankings of causes of death. There could be differences in the top 10 causes of deaths between males and females and between both countries. There are a number of reasons for these differences SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 98 between countries including political, economic, social contexts as much as biological susceptibility or climatic conditions (Birn, Pillay & Holtz, 2008: 245). 3. DALYs provide a richer picture of disease because they add the burden of non-fatal disease such as mental health problems, e.g. depression, which would previously not have been captured by using mortality data alone. 5.4 Subsequent BOD Studies Subsequent to the 1990 GBD study, a number of countries conducted BOD studies, some of the first being Mexico, Australia, the Netherlands and the USA. Although it is often challenging to access mortality and morbidity data in most African countries, a number of countries have conducted BOD studies including Zimbabwe, Uganda, South Africa. Although each of these countries has used the GBD classification and methodology they have adapted it for their own country. For example, a BOD study was conducted in South Africa in 2000 (10 years later). Look at Figure 3.4 below. Figure 3.4: The top 20 causes of death and YLL for South Africa in 2000. (Source: Bradshaw et al., 2003: 37) LISTEN TO INTERVIEW ON YOUR PG DIPLOMA CD Now listen to an interview with Prof Debbie Bradshaw of the Medical Research Council of South Africa which you will find on your CD. Hazel Bradley interviewed her about her experience of undertaking the BOD study in South Africa. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 99 TASK 8 – Listen to an interview with questions in mind To improve your listening, try to find answers to these questions as you listen. 1. Can you give us a bit of background to the study? When was it undertaken, why, by whom, and how? 2. Have any other African countries done the same? 3. Can you share some of your experiences and challenges in developing of the BOD study in South Africa 4. Can you tell us how BOD studies are being used in South Africa? 5. And finally is it an ongoing process and where can you get BOD information by country, particularly for sub-Saharan countries? 6. What contributions do DALYs make to understanding the burden of disease in these countries? FEEDBACK Now that you’ve heard the interview, find out whether any such study has been undertaken in your country or region. From question (4) above, you might now have some ideas of the value of BOD studies. But let us explore this question a little further. 5.5 The value of BOD studies There are five main ways in which BOD studies are helpful in the formulation of health policy: to help assess performance of one country or to compare performance of different countries; they provide a forum for debating the disease burden; they help establish a shortlist of disease control priorities; Establishing research and development priorities; Allocating resources across Health Interventions. These are further discussed on this website: [Online], Available: http://www.dcp2.org/main/Home.html, where a book called Priorities in Health Project is provided. Explore the site and see what else is available on it. In conclusion, the GBD study and the studies which have followed have added a number of dimensions to understanding the health of populations. First of all, they highlight key areas for preventive interventions, and as Lucas and Gilles (2004: 20) note, “they are increasingly being used to make objective decisions for setting priorities in the health sector”. DALY’s as a measure are also helpful in highlighting the health services required to manage these diseases because they emphasize and incorporate the burden placed by morbidity. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 100 Finally, they also emphasized that the burden of neuropsychiatric diseases and injuries were vastly under-appreciated when health was measured by mortality alone. 6 COMPARATIVE RISK ASSESSMENT (CRA) The next stage in the BOD work was to estimate the contribution of various risk factors to morbidity and mortality. The value of doing this is that understanding risks to health is critical in preventing disease and injury. In particular, it can guide us to the type of interventions that can be made to improve health. If we can quantify the impact of various risk factors on diseases, this can assist us in deciding on the most important interventions to focus on. Before going any further, we should clarify the concept “risk factor” which you will be expected to use in your discussions of disease. Vaughan and Morrow (1998) note that it is used in two different ways: (1) (2) an attribute, variable or exposure that is associated with an increased probability of a specified event, such as occurrence of a disease. Such preceding factors are not necessarily causal (also called risk markers); an attribute, variable or exposure that actually increases the occurrence of a specified event, and is therefore believed to be causal (also described as a determinant) (Vaughan & Morrow, 1998: 165) Global Health Risks on the other hand are defined as follows: A particular disease or injury is often caused by more than one risk factor, which means that multiple interventions are available to target each of these risks. For example, the infectious agent Mycobacterium tuberculosis is the direct cause of tuberculosis; however, crowded housing and poor nutrition also increase the risk, which presents multiple paths for preventing the disease. In turn, most risk factors are associated with more than one disease, and targeting those factors can reduce multiple causes of disease. For example reducing smoking will result in fewer deaths and less disease from lung cancer, heart disease, stroke, chronic respiratory disease and other conditions” (WHO, 2009:1) There are two main approaches to reducing risk: Targeting high-risk people, who are most likely to benefit from the intervention Targeting risk in the entire population The comparative risk assessment (CRA) methodology developed by WHO is a standardized and systematic approach to estimating the contribution of risk factors to the BOD. In 2009 the WHO published the Global Health Risks Report which provided information on the CRA for 2004 for 24 global risk factors. The study found that over SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 101 one third of the world’s deaths could be attributed to only 10 risk factors and that 44% of global deaths and 34% of DALYS could be attributed to the 24 risk factors. The tables below show the 10 leading risk factor causes of death and DALYS for the world and by income group. Take a few minutes to study these two tables. Firstly notice the similarities and differences between the four groups, (that is world, lowincome countries, middle income countries and high income countries) in each table and then look at the similarities and differences between the two tables (that is death and DALYS). Tables from WHO. (2009). Global Health Risks. A Response to the Need for Comprehensive, Consistent and Comparable Information on Health Risks at Global and Regional Level. [Online], Available: http://www.who.int/mediacentre/news/releases/2009/health_risks_report_20091027/en/ index.html [Downloaded: 17.1.10]. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 102 You will notice that the top 10 risk factors in the world vary according to income group. The top five risk factors globally are high blood pressure, tobacco use, high blood glucose, physical inactivity and overweight and obesity. These are responsible for increasing chronic diseases, like heart disease. These affect all income groups. Now look at the second table which shows the leading risk factor causes of DALYS. (Remember that DALYS is a measure that gives more weight to non-fatal loss of health and deaths at younger ages.) Here you will notice that the top five risk factors globally are underweight, unsafe sex, alcohol use, unsafe water and high blood pressure. Three of these top five risks relate to communicable diseases and affect mainly low income countries. Although the global assessment of risk factors gives an indication of risk factors to be addressed, a national assessment provides more useful information on the impact of key risk factors on health. In 2007, South Africa published its first Comparative Risk Assessment in which the contribution of 17 selected risk factors to the burden of disease in 2000 was estimated. Read this article and complete the session by doing the final Task. Note: We do want you to spend too much time on the methodological details, but rather to gain a grasp of the concepts of CRA and its value and use in Public Health. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 103 READING Norman, R., Bradshaw, D., Schneider, M., et al. (2007). A Comparative Risk Assessment for South Africa in 2000: Towards Promoting Health and Preventing Disease. South African Medical Journal, 97: 637-641. TASK 9 – Understand Comparative Risk Factor Assessment 1. For practice, see whether you can download this reading from the Medical Research Council website by typing the URL http://www.mrc.ac.za into your search engine. Then click on “Research”, and look under “Health Priorities for Public Health”. Listed under “Research Units and Lead Programmes”, click on “Burden of Disease Research Unit”. Then click on “Outputs and briefs” and look under “Latest releases”. There you will find: “17 Risk factors”. Click on the link to the pdf of the publication in the SAMJ in August 2007. 2. Explain how the 17 risk factors used in the CRA for South Africa were selected. 3. Note the top five risk factor causes of death for South Africa listed in Table 1 of this reading and compare them with the top five risk factors of the global and three income groups in Table 1 of the Global Health Risk Report. 4. What does the leading risk factor for cause of death South Africa in the table tell you about the burden of disease for South Africa in 2000? 5. How have the authors proposed that the South African CRA can be used? FEEDBACK 1. The risk factors were selected on the following basis: the burden of disease in South Africa; input from stakeholders including the Department of Health; a list of criteria: i. likely to be among the leading causes of burden of disease and injury ii. evidence of causality iii. potentially modifiable iv. availability of data; focused on direct physiological and environmental risks rather than underlying factors such as poverty and social inequality. 2. In the South African CRA, the leading 5 risk factor causes of death were: Unsafe sex/STIs High blood pressure Tobacco smoking Alcohol harm High BMI. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 104 3. With the exception of the top risk factor – unsafe sex and STIs, they match most closely to the middle-income countries group. This is understandable as South Africa is classified as a middle income country. 4. The leading risk factor, unsafe sex/STI is responsible for over ¼ of the total deaths in 2000. The underlying disease attributed to this risk factor in HIV/AIDS. The huge number of deaths that were due to HIV/AIDS in South Africa in 2000 have contributed to this being the leading risk factor. 5. The SA CRA has highlighted the health impact of major risks on the health of the population. The authors say that this information provides the government with information it needs to introduce policies and strategies to address the major risk factors identified by the CRA. 7 SESSION SUMMARY This session has introduced you to some important considerations regarding populations and health – the Health Transition and the Global Burden of Disease studies. You have also been guided to accessing this kind of information and to the nature and value of Comparative Risk Assessment. We hope you have found the session interesting, and will take a well-deserved break before moving onto the Group 1 diseases – Communicable Diseases. 8 REFERENCES AND FURTHER READING Beaglehole, R. & Bonita, R. (2001). Public Health at the Crossroads: Achievements and Prospects. Auckland, New Zealand: Cambridge University Press. Birn, A-E., Pillay, Y. & Holtz, T. H. (2009). Textbook of International Health: Global Health in a Dynamic World. New York/Oxford: OUP. Bradshaw, D., Groenewald, P., Laubscher, R., Nannan, N., Nolijana, B., Norman, R., Pieterse, D. & Schneider, M. (2003). Initial Burden of Disease Estimates for South Africa, 2000. Cape Town: MRC. Bradshaw, D. Ch 15 - Burden of Disease and Mortality Studies. G. Joubert & R. Ehrlich with J. Katzenellenbogen & S. Abdool Karim (eds). (2008). Epidemiology: A Research Manual for South Africa. 2nd ed. Cape Town: Oxford University Press. Feachem, R. G. A., Kjellstrom, T., Murray, C. J. L., Over, M. & Phillips, M. A. (1991). SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 105 Frenk, J., Bodadilla, J. L., Sepúlveda, J., & Cervantes, M. L. (1989). Health Transition in Middle-income Countries: New Challenges for Health Care. Health Policy and Planning, 4: 29-39. Friis, R.H. & Sellers, T.A. (2004). Epidemiology for Public Health Practice. Sudbury, MA: Jones & Bartlett. Joubert, G. & Ehrlich, R. with Katzenellenbogen, J. & Abdool Karim, S. (2008). Epidemiology: A Research Manual for South Africa. 2nd ed. Cape Town: Oxford University Press. A. D. Lopez, C. D. Mathers, M. Ezzati, D. T. Jamison & C. J. L. Murray (eds). (2006). Global Burden of Disease and Risk Factors. New York: Oxford University Press. Montgomery, K. The Demographic Transition. Dept of Geography and Geology. [Online], Available: //http:www.uwmc.uwc.edu/geography/Demotrans/demtran.htm [Downloaded: 15.1.10]. Omran, A. R. (1971). The Epidemiologic Transition: A Theory of the Epidemiology of Population Change. Milbank Memorial Fund Quarterly, 49: 509-538. Olshanky, S. J. & Ault, A. B. (1986). The Fourth Stage of Epidemiologic Transition: the Age of Delayed Degenerative Diseases. Milbank Memorial Fund Quarterly, 64: 355-391. Vaughan, J.P. & Morrow, R.H. (1998). Manual of Epidemiology for District Health Management. Geneva: WHO. Walley, J., Wright, J. & Hubley, J. (2001). Public Health: An Action Guide to Improving Health in Developing Countries. Oxford: Oxford University Press. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 106 Unit 2 – Session 3 Communicable Diseases Introduction In this session, we will introduce the first group of diseases outlined in Session 1, namely communicable diseases. Although communicable diseases can occur in any population, they predominate in poorer communities and in lower income countries (Walley, Wright & Hubley, 2001). Preventing and controlling them is a key strategy in improving health in the developing world. Although the extent or impact of some communicable diseases has been significantly reduced through strategies such as immunisation – and in the case of smallpox, a disease has been eradicated - other have emerged or re-emerged. Examples of new and re-emergent infectious diseases include HIV/AIDS, hepatitis C, multi-drug resistant tuberculosis, SARS, and others. HIV/AIDS has caused huge mortality and disease burden in some countries, particularly those in sub-Saharan Africa, with reversals of gains in life expectancy that had been won over the previous decades. Different professionals in the health team need different information about a disease according to the role they play in the field. As a Public Health worker, you are not expected to know every last detail of every communicable disease; however, it is important to understand where to find information should you need it, what aspects to focus on, and above all, to understand prevention and control strategies at the population level. If you are trying to prevent the spread of a disease, you need to understand how it is spread, prevented, managed and controlled. Chapters 4–7 of the setwork in Lucas and Gilles (2004) reading focus on communicable diseases, so this is one ready reference. This session will bring together in a shorter form some of the major concepts and frameworks used in Public Health approaches to communicable diseases and discussed in the readings. Contents 1 2 3 4 5 6 7 8 9 Learning Outcomes of this Session Readings Communicable disease in the global context A Public Health perspective on Communicable Diseases Frameworks for understanding Communicable Diseases Control of Communicable Diseases Additional resources Session summary References and further reading SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 107 1 LEARNING OUTCOMES OF THIS SESSION By the end of this session, you should be able to: 2 Demonstrate understanding of a range of key concepts in relation to selected communicable diseases. Explain why a public health practitioner needs to understand the biological basis of communicable diseases. Explain the biological basis of communicable diseases and their risk factors. Apply models of infection to a range of diseases, e.g. chain of infection, or host, agent and environment. Demonstrate familiarity with scholarly sources of information on communicable diseases. Demonstrate familiarity with prevention and control measures for communicable diseases. READINGS The readings for this session are listed below. You will be directed to them in the course of the session. Author/s Publication Details World Health Organisation (Health Statistics and Informatics Department) Friis, R.H. & Sellers, T.A. Lucas, A. O. & Gilles, H. M. Nelson, K. (2004), Global Burden of Disease 2004 Update: Selected Figures and Tables. Geneva: WHO. [Online], Available: http://www.who.int/healthinfo/global_ burden_disease/2004_report_update/en/index.html [Downloaded 17 1 10]. On your DVD: GBD 2004 Report Figures (2004). Ch 12 – Epidemiology of Infectious Diseases, Epidemiology for Public Health Practice. Sudbury, MA: Jones & Bartlett: 398–411. (2004). Ch 3 – Epidemiology. Short Textbook of Public Health Medicine For the Tropics. London: Arnold Publishers: 29–47. Setwork (2007). Introduction to Infectious Disease Epidemiology. Johns Hopkins University: Slides 43 – 63. On your DVD: Intro Infectious Disease Epi SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 108 3 COMMUNICABLE DISEASE IN THE GLOBAL CONTEXT TASK 1 – Define communicable disease 1. Before we start, jot down your own definition of communicable diseases and infectious diseases. Now list three examples of each. Take a look at page 35 of Lucas and Gilles (2004), where they characterise communicable disease. 2. A number of books, including your setwork, use the term “infectious diseases”. What is the difference between the two? FEEDBACK Communicable diseases are characterised by the existence of a transferable living infectious agent; in other words, the disease can be transferred from one host to another by an agent of some kind. Infectious disease is defined in Last’s dictionary (2001) as “an illness due to a specific infectious agent or its toxic products that arises through transmission of that agent or its products from an infected person, animal, or reservoir to a susceptible host, either directly or indirectly, through an intermediate plant or host, vector, or the inanimate environment” (Joubert & Ehlrich, 2008: 221). For practical purposes, these two terms are fairly close, although strictly speaking some infectious diseases might not be communicable from one person to another. Now let’s link communicable diseases with the global burden of disease which was discussed in the last session. READING WHO. (Health Statistics and Informatics Department). Global Burden of Disease 2004 Update: Selected Figures and Tables. Geneva: WHO. [Online], Available: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.htm l [Downloaded 17 1 10]. Look for: GBD 2004 Report Figures on DVD. TASK 2 – Refresh your understanding of the GBD Look at the above powerpoint presentation on your DVD in the GBD2004Reportfigures. Slide 15 shows the burden of disease by broad cause group and region for 2004. 1. List the six regions into which the global population is divided. 2. How is the disease burden measured in the GBD report? Explain this measure. 3. What is the total disease burden for the Africa region? Compare this to the other five regions. 4. What conditions account for the highest proportion of the BOD in the Africa region? SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 109 FEEDBACK 1. See slide 11. 2. DALYs. See Unit 2 Session 2, section 5.2 for an explanation. 3. In the Africa region, the total disease burden in DALYs is about 500 per 1 000 population, which is much greater than any of the other regions five regions. See Slide 14. 4. You will see on Slide 14 that Group I causes - communicable diseases, maternal, perinatal and nutritional conditions - form the largest proportion of the burden of disease in the Africa region. 4 A PUBLIC HEALTH PERSPECTIVE ON COMMUNICABLE DISEASE You may be familiar with diseases from a clinical perspective, however there are other ways of looking at disease which serve purposes other than diagnosing and treating (and hopefully curing!) an individual. The clinician is trained to consider disease from the perspective of its signs and symptoms. For example, many countries have implemented the Integrated Management of Childhood Illnesses (IMCI) Programme which has a problem-based approach to the management of health conditions in children presenting at community and Primary Health Care (PHC) level. If a child is identified in the community or presents at a primary care facility with diarrhoea, then the health worker will take a history, carry out a clinical examination, make an assessment and recommend treatment based on the severity of the signs and symptoms. On the other hand, the microbiologist’s role is to investigate the different causes of diarrhoea and the possible infectious agents and to understand and classify disease it in terms of its biology. She or he looks at the disease in terms of the infectious cause, i.e. the microbe. A third perspective is one that we hope you will develop in the course of this programme, as you move towards developing your role as a Public Health professional - from an epidemiological viewpoint. If the same child were considered by a Public Health worker, they should raise concern about how the child became ill, and whether the child is part of a bigger trend in the community. In broad terms an epidemiologist is interested in the distribution and causes of disease, as well as prevention and control methods. As a Public Health professional, you need a basic understanding from all these perspectives, but the epidemiological perspective is especially important in Public Health and in understanding communicable diseases. The key message here is that in order to prevent communicable diseases and to manage and control them where they occur, the Public Health professional needs to understand them in detail. You have already read a little about epidemiology, and the role of the epidemiologist, but let us discuss who plays this role a little further. Although the state health department and a number of parastatal medical research units employ epidemiologists SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 110 to monitor disease, conduct surveillance, and assess outbreaks and epidemics when they occur, there is a much wider group of people who need to have a broad understanding of the distribution and causes of disease in populations. Public Health professionals, however, need to be able to read epidemiological reports, graphs and data, and to interpret data and act on epidemiological findings. This is what you will learn to do in your third module – Descriptive Epidemiology; here however you will be exposed first and foremost to communicable diseases through to epidemiological information. Epidemiologists are interested in the distribution of diseases in the population, against the background of their environment. So, in addition to the infectious agent itself, epidemiologists are interested in other aspects that influence the spread of infectious diseases including the host, environment, reservoir, route of transmission. Epidemiologists need to understand the role of each of these in communicable diseases. TASK 3 – Compare the information needed by three different health professionals 1. Develop a table comparing the kinds of information a clinician, a microbiologist and an epidemiologist needs to know about malaria. Clinician Signs and symptoms Microbiologist Epidemiologist 2. Why does the epidemiologist or Public Health professional need to understand these aspects of malaria? FEEDBACK 1. A comparison of the information needed by three groups of health professionals: Clinician Signs and symptoms Susceptibility Treatment Consequences and burden on the population Microbiologist Causes Classification of infectious agents Mode of transmission (agents, vectors, reservoir) Epidemiologist Prevalence of this health problem within the context population susceptibility Mode of transmission (agents, vectors, reservoir) Incubation period Consequences and burden on the population Prevention/Methods of control 2. A Public Health professional/epidemiologist needs to understand these aspects of malaria because her or his role is to control the further incidence of malaria by managing the vectors of transmission (mosquitoes) and the population’s ability to SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 111 protect themselves from malaria. Furthermore, these professionals need to know about the impact of the disease, its incubation period, how the disease has been controlled in the past and whether there are any new strategies that have been tested and might be adapted for the local context. 5 FRAMEWORKS FOR UNDERSTANDING COMMUNICABLE DISEASES In this section, we will introduce a number of concepts and ways of thinking about communicable disease that have proven useful in public health practice. These concepts and frameworks are discussed in your readings, and are summarised here in a more condensed way. We have noted that epidemiologists are interested in the distribution of diseases in the population, against the background of their environment. So, in addition to the infectious agent itself, epidemiologists are interested in factors that influence the spread of infectious diseases. These include the host, the environment, what is called the “reservoir”, and the route of transmission. Epidemiologists and Public Health professionals need to understand the role of each of these elements in order to be able to grasp a broader picture of the spread of communicable diseases. The Epidemiologic Triangle A model that has been widely used for many years to explain the pathogenesis of communicable diseases is the epidemiologic triangle or triad. It demonstrates the relationship of the disease, the host, the agent and environmental factors. “[It] …provides one of the fundamental public health conceptions of disease causality” (or etiology) (Friis & Sellers, 2004: 398). As a Public Health practitioner it is critical that you have a good understanding of the interaction of the three components of the triad in relation to each disease in order to fully understand the process of infection and to understand the role of each element in the chain of infection. This is the key to Public Health practice when it comes to preventing communicable diseases. Pathogenesis The propensity for an agent to cause disease or clinical symptoms measured by the apparent: inapparent infection ratio. READING Friis R. H. & Sellers T. A. (2004). Ch 12 – Epidemiology of Infectious Diseases. Epidemiology fro Public Health Practice. Sudbury: Jones and Barlett: 397–411. Read up to the end of the section on “Means of Transmission – Directly or Indirectly from reservoir” on page 411. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 112 The Epidemiologic Triangle HOST AGENT ENVIRONMENT For infection to take place, the presence of the infectious agent is necessary as well as a susceptible host and a conducive environment. After exposure the host progresses through a chain of events from sub-clinical (inapparent) infection to an active case of the disease: the result may be complete recovery, disability or death. The occurrence and outcome of infection is affected by a number of factors, some of which are determined by the host, others by the environment, others by the agent, and yet others by interactions among these. Host Factors These include the host’s ability to resist or fight the infectious agent. Resistance of the host, or immunity, is affected by a range of both non-specific and specific (to the particular disease) factors including – age, sex, pregnancy, nutritional status, trauma and fatigue and herd immunity, as well as specific individual antibodies or other immune responses to a particular infectious agent. You can read more about these in Lucas & Gilles (2003: 38-39.) TASK 4 – Explore the host’s defence mechanisms 1. Develop a table of the non-specific and specific defence mechanisms that the human body (host) may exert to resist the infection. You will find some information about this in the Friis & Sellers (2004) reading and in your setwork by Lucas and Gilles (2003) in Chapter 3. Non-specific defense mechanisms Specific defense mechanisms SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 113 Environment The environment refers to the domain in which the infectious agent may exist, survive or originate. It includes the physical, climatologic, biologic, social and economic components which play a critical role in the development of communicable diseases. The environment may act as a reservoir for the infectious agent and includes human reservoirs, animal (zoonoses) or insect reservoirs (vectors) and environmental reservoirs such as water, soil or food. Agent The third point of the triangle is the one that most readily comes to mind – the actual infectious agent (bacterium, virus, protozoan, etc) that “causes” the disease. The importance of the epidemiological triangle is to remind us that an agent on its own does not actually create disease: a susceptible host and a conducive environment (from the perspective of the agent, that is!) are equally necessary. Look at the presentation on your DVD and focus on slides 56 – 59. READING Nelson, K. (2007). Introduction to Infectious Disease Epidemiology. Johns Hopkins University. On DVD: see slides 56–59. Look for Intro to Infectious Disease Epi on DVD. TASK 5 – Clarify concepts 1. Develop a concept list from the above reading, in which you define the following key concepts: infection, agent, host, vehicle, vector, reservoir. You will need to look up some of these concepts on the web. 2. Classify the following communicable diseases by microbial infectious agent: schistosomiasis candidiasis tuberculosis hepatitis A malaria tapeworm trypanosomiasis influenza salmonellosis 3. Infectious disease agents a) Name two diseases which have high infectivity: b) If an agent is able to survive poor environmental conditions, it is said to be … c) If the rabies agent is said to be virulent, what does this mean? d) Write a paragraph describing the concept of the environment in relation to disease. e) What is meant by: Infectivity: Pathogenicity: Virulence: SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 114 FEEDBACK 1. Key concepts defined: Infection Infection is the entry and multiplication of an infectious agent in the host and is not the same as clinical disease. Infection does not always lead to disease, or signs and symptoms of ill-health. Agent The infective organism: a variety of microbial agents or organisms exist including viruses, bacteria, mycoses or fungi, protozoa, helminths and arthropods which trigger infection. An agent must be present for an infectious disease to occur. Characteristics of infectious agents In order to survive the infectious agent must be able to: Multiply Emerge from the host Reach a new host Infect the new host However some infectious agents cause disease through the toxins they produce. For example, some kinds of food poisoning are caused not by the bacterium that is ingested, but by the toxins that the bacterium has produced and left in the food that is eaten. In addition there are a number of characteristics that influence whether an infectious agent will produce disease in a host and the severity and outcome of the disease. These include infectivity, pathogenicity and virulence. Host Susceptible persons – the infection is affected by the host’s resistance manifest by non-specific and disease-specific defense mechanisms. Vehicle The route of transmission Vector Any arthropod or animal which carries and transmits infectious pathogens directly or indirectly from an infected animal to a human or from an infected human to another human (Friis & Sellers, 2004: 345) Reservoir Any person, animal, arthropod, plant or soil in which an infectious agent lives and multiplies. 2. schistosomiasis - helminths candidiasis - mycoses tuberculosis - bacteria hepatitis A - virus malaria – protozoa = infectious agent; arthropods = vectors tapeworm - helminths trypanosomiasis – arthropods = vectors influenza - virus SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 115 salmonellosis - bacteria 3. Infectious disease agents a) Measles and polio b) If an agent is able to survive poor environmental conditions, it is said to be resistant. c) If the rabies agent is said to be virulent, it causes severe illness. In the case of rabies, once the disease occurs, it is almost always fatal. d) Some key points might be: it may include physical, climatic, social, biological and economic aspects; the environment can serve as a reservoir for the infective agent, e.g. contaminated water; or a human may be the reservoir host, e.g. for smallpox, or an arthropod may be the environment or vector for infection. e) Infectivity: capacity of agent to enter host and cause infection or disease. Pathogenicity: capacity of agent to cause disease in host. Virulence: severity of disease. (See slide 60 Johns Hopkins) TASK 6 – Apply the epidemiologic triangle 1. Explain the etiology, or causality, of tuberculosis, constructing an epidemiologic triangle. 2. Identify the reservoirs for these diseases: rabies measles pseudomonas infections salmonelosis tetanus HIV/AIDS botulisim gonorrhea FEEDBACK 1. Tuberculosis HOST FACTORS: Non-immune, weakened resistance, poor nutrition, concurrent disease (e.g. HIV) AGENT: Mycobacterium tuberculosis ENVIRONMENTAL FACTORS: crowded conditions, poor ventilation SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 116 2. Reservoirs of infectious diseases: typhoid fever - human rabies – animal (zoonoses) measles - human pseudomonas infections – water salmonelosis – human and animal tetanus - soil HIV/AIDS – human botulisim - soil gonorrhea - human Variations in severity of the infection In relation to infection, the variations in severity of the infection are conceptualised along a spectrum from inapparent infection, e.g. with tuberculosis to severe and fatal infection. See Figure 12.3 on page 403 in Friis and Sellers (2004) reading. Transmission of infectious disease Transmission is the mechanism by which an infectious agent is transmitted through the environment to another person. Transmission may be direct or indirect Direct transmission This includes infectious diseases spread by direct person to person contact. This may happen in a number of ways: touching (for example for some skin diseases), airborne particles or droplets (through coughing or sneezing - tuberculosis), kissing (mononucleosis), sexual intercourse, childbirth, breast feeding, blood transfusion or blood contact through injury, or transplacental transmission (HIV). Indirect transmission This involves the spread of infectious diseases through an intermediary source: this includes Vehicles - food, water, air Vectors -insects or animals Fomites - inanimate objects, e.g. door handle, clothing, dirty needles and syringes. Sometimes infectious diseases are classified into broad categories such as waterborne, food borne, arthropod-borne, vaccine. Look at Figure 12-2 on page 400 in Friis and Sellers (2004) reading. TASK 7 – Answer a critical question 1. How will knowing how an infection is transmitted assist you in selecting control methods? SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 117 FEEDACK 1. Direct transmission can be interrupted by controlling the source, but indirect transmission requires a different approach, such as the use of mosquito nets or correct food storage conditions. We will cover more about control of communicable diseases later in this session. Chain of infection On page 406 of Friis and Sellers (2004) is another classic model for explaining communicable diseases – Figure 12-4 The chain of infection. It illustrates the process of transmission. This diagram illustrates the stages involved in transmission of an infectious disease and includes both direct and indirect transmission. Figure 12-4: The chain of infection (Friis and Sellers, 2004: 406) Source: DVDC. (1998). Principles of Epidemiology. Atlanta GA. Portals of entry and exit are included in the diagram and are the sites where infectious agents enter and leave the body, e.g. through insect bites or accidents. The infectious agents are transmitted in various ways and then enter the susceptible host through portals of entry. Table 12-1 on page 407 (Friis and Sellers 2004) illustrates relationship between portals of exit, mode of transmission and portal of entry of a number of infectious diseases. You may have noticed that the textbook we have recommended by Lucas and Gilles organises communicable disease by their portals of entry into the body. So Chapter 4 covers infections through the gastro-intestinal tract; Chapter 5 covers infections through skin and membrane; Chapter 6 covers infections through respiratory tract and Chapter 7 covers arthropod-borne infections. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 118 6 CONTROL OF COMMUNICABLE DISEASES Control of communicable diseases must be based on knowledge and understanding of the epidemiology of the infection, which we have been covering in this session and public health principles. There are three main strategies for controlling communicable disease: the choice depends on which strategy is likely to be most effective and most feasible for a particular disease in a particular setting or context. The strategies are: 1. Eliminate reservoir of infection 2. Interrupt the pathway of transmission 3. Protect susceptible hosts TASK 8 – Identify the control of communicable diseases Identify how to control communicable diseases. Some of the key points have been summarised below and we have left some spaces for you to fill in the gaps in your own words from sources you have read. Look at the sections in your setwork (Lucas & Gilles pages 42–45) and other texts. 1. Elimination of reservoir We have already mentioned earlier in this session that agents live in different reservoirs. Look at Slides 55–59 to refresh your memory of the different reservoirs and examples of some of the infective agents. Eliminating the reservoirs is one way of eliminating the infectious agent and controlling the communicable disease. (Fill in the gaps in your own words.) Human reservoir Animal reservoirs (Zoonoses) Non-living reservoir Water Soil 2. Interruption of transmission SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 119 This usually includes improvement in the environment such as providing clean water and adequate sanitation. Control of vectors such as mosquitos depends on altering the environment or use of pesticides, such as spraying inside homes. Another example of vector control: 3. Protection of susceptible host An established way of controlling communicable disease is by protecting individuals from infections. Protection may be by immunisation or by drugs. Fill in the gaps in your own words. Immunisation Passive immunisation Active immunisation Routine immunisation Routine immunization of children against diphtheria, pertussis tetanus, measles, poliomyelitis and other diseases is an important way of controlling these infections and improving child health. The WHO Expanded Programme on Immunization (EPI) assists developing countries with immunization programmes. You can find out more information on EPI by searching the WHO website (www.who.int). Vaccines can also be used to control outbreaks of diseases, for example measles outbreak. Find out the current EPI schedule for your country: Drugs Drugs can be used to treat individual patients, such as the use of antibiotics for bacterial infections. However, they may also be used to reduce the risk that being exposed to infection will lead to disease. For example, travellers visiting areas where malaria is endemic may take anti-malarial drugs. These do not prevent malarial parasites from entering the body (which is what insect repellent and bednets seek to do), but they prevent the replication of the agent to the level where disease occurs. Other examples of using medications to control or prevent communicable disease (“prophylaxis”) include the use of antibiotics to prevent some kinds of pneumonia in people living with HIV. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 120 TASK 9 – Develop a Fact Sheet You may need to develop a series of Fact Sheets for health workers in your district (one that is suitable for both health professionals such as doctors and nurses and also community health workers) on a number of communicable diseases. 1. Choose one disease and draft an outline of such a Fact Sheet. 2. Use the following sub-headings: Clinical features – signs and symptoms Agent Incubation period Incidence of this health problem within your district (Choose one of your districts) Mode of transmission (agents, vectors, reservoir) Population at risk Treatment Consequences and burden on the population Prevention/Methods of control The information on your Fact Sheet may be the starting point for Assignment 2. 7 ADDITIONAL RESOURCES You may find the following resources helpful to you, bearing in mind that there is much more than this. WHO website http://www.who.int WHO Facts sheets: http:// www.who.int/mediacentre/factsheets Johns Hopkins Open Courseware: http://ocw.jhsph.edu/ American Public Health Association: http://www.apha.org/ Open Courseware Consortium: http://www.ocwconsortium.org/use/use-dynamic.html Centers for Disease Control and Prevention: http://www.DVDc.gov/ The International Development Research Centre: http://www.idrc.ca/en/ev-1-201-1DO_TOPIC.html 8 SESSION SUMMARY We started off this session by drawing your attention to the huge burden of communicable diseases in low-income countries and sub-Saharan Africa, in particular. We have ended by looking at measures of prevention and control of communicable diseases and this, of course, is key if the number of people suffering from communicable diseases is to decrease. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 121 We hope that in-between you have become acquainted with the main facts about a range of the most common communicable diseases. Finally, as you think about applying control of communicable disease strategies in your country, reflect back to Unit 1 Session 1 where you were introduced to the concepts of health promotion and disease prevention. Whilst most of the preventive strategies fall under the remit of the health services, promotive activities are generally broader – involving sectors other than health and often involve policy and legislation. Social, economic and environmental determinants play a critical role and this is another reason why the Public Health practitioner must have a broad understanding of health and its determinants and work closely with a wide range of role players in improving population health. 9 REFERENCES AND FURTHER READING Walley, J., Wright, J. & Hubley, J. (2001). Public Health: An Action Guide to Improving Health in Developing Countries. Oxford: Oxford University Press. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 122 Unit 2 – Study Session 4 Non-communicable Diseases Introduction Chronic diseases are often characterised as problems of affluence, of ageing communities who have acquired them through indulging in the risk factors for disease (tobacco use, unhealthy diets, and physical inactivity). This view is inaccurate: chronic disease is a larger problem in low-income countries, especially among those who do not have the resources to pursue healthy choices easily. (Strong, Mathers, Leeder & Beaglehole, 2005: 1581) As Lucas & Gilles (2003) point out, “… the past few decades have seen significant changes in the pattern of health and diseases. These changes are the result of social, economic and technological developments, as well as specific public health and population programmes in developing countries.” Lucas & Gilles (2003) continue: “As communicable diseases, malnutrition, and problems associated with pregnancy and childbirth have come under control, chronic, non-communicable diseases (NCDs) have replaced them as the dominant Public Health problems.” In previous study sessions we have noted that some countries, including South Africa, still have a high burden of communicable diseases and HIV/AIDS, as well as an increasing burden of non-communicable diseases and injuries. You may remember that this has been called the triple, even quadruple burden of disease. In this session we focus on non-communicable diseases and in the session that follows, injuries. The burden of NCDs continues to rise globally and constitutes one of the major challenges in the 21st century. In 2005, for example, NCDs caused an estimated 35 million deaths which represents 60% of all deaths globally; of these, 80% of deaths occurred in low and middle income countries. The total number of deaths from NCDs is projected to rise by 17% over the next 10 years (WHO, 2008). Despite these statistics pointing to an increasing global NCD problem, and evidence that poor and disadvantaged populations are disproportionately affected, NCDs have been somewhat marginalized on the health agenda. Instead, the last few years have seen a global and local focus on priority diseases – HIV/AIDs, TB and malaria through global initiatives such as the Global Fund for the Prevention of TB, HIV and Malaria, which have ploughed huge amounts of funding into programmes in developing countries. Further evidence of the marginalization of NCDs is that even the Millennium Development Goals (set in 2000) do not address NCDs specifically at all. This lack of SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 123 urgency on non-communicable diseases has been a concern for researchers in the field for some time now; and in response, the WHO recently launched a Global Strategy for the Prevention and Control of Non-communicable Diseases: Action Plan, 2008-2013. Contents 1 2 3 4 5 6 Learning outcomes for this session Readings Non-communicable diseases and their risk factors Responding to the challenges of NCDs Session summary References and further reading 1 LEARNING OUTCOMES OF THIS SESSION By the end of this session, you should be able to: 2 Explain key concepts in relation to a range of non-communicable diseases. Demonstrate an understanding of the risk factors for non-communicable diseases. Demonstrate an understanding of the role of social determinants on noncommunicable diseases. Present evidence of familiarity with prevention and control measures for noncommunicable diseases. READINGS Author/s Beaglehole, R., EppingJordan, J., Patel, V., Chopra, M., Ebrahim, S., Kidd, M. & Haines, A. Publication Details (2008). Improving Prevention and Management of Chronic Disease in Low-income and Middle-income Countries: A Priority for Primary Health Care. Lancet, 372: 940–949. Lucas, A. O. & Gilles, H. M. (2003). Ch 8 – Non-communicable disease: Health in Transition. Short Textbook of Public Health Medicine for the Tropics. 4th ed. London: Arnold Publishers: 235–236. Puoane, T., Tsolekile, L., Sanders, D. & Parker, W. (2008). Chronic non-communicable diseases. South African Health Review. Durban: Health Systems Trust: 73–87. Also SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 124 available [Online]: http://hst.org.za/uploads/files/cont_ack_08.pdf Downloaded: 03 / 12/09 3 NON-COMMUNICABLE DISEASES AND THEIR RISK FACTORS The following quotes come from respondents in a study conducted in Cape Town, South Africa by Sengwana & Puoane (2004); various studies have found such quotes to reflect some of the prevailing attitudes and beliefs towards non-communicable diseases, and their attendant risk factors, in a low-income community in a developing country. “Almost every adult in the community is on treatment for hi-hi (hypertension). People are surprised to meet someone above 50 years who is not on treatment for hypertension. It is just like overweight, almost all women in the community are overweight.” (Sengwana & Puoane, 2004: 67) “We understand hypertension is a disease common in overweight people, but we also see thin people who adhere to healthy living (these people were considered not at risk) with no family history of hypertension, but told that they suffer from hypertension. Most people think that hypertension is therefore caused by witchcraft.” (Sengwana & Puoane, 2004: 67) “People are not concerned about hi-hi, because of poverty. They worry about what they are going to eat… people are depressed about their poverty situation and some are very stressed... people are not working and this forces them to eat whatever is available You may find that one person in the house has diabetes or hypertension but cannot control her diet because the little food available has to be shared with the whole family.” (Sengwana & Puoane, 2004: 67) CASE STUDY Setting Khayelitsha is a residential area of Cape Town which is characterized as a “township” – a term which, in South Africa, refers to historically “black” residential areas in the urban areas. Khayelitsha was established and grew over the 1980s, with large numbers of residents coming from their rural home areas to seek work and to escape rural poverty. The population was ill provided for when they settled: some residents built shacks and recreational facilities were scarce and crime levels high. The City Council has been slow to provide water and sanitation and food shopping amenities. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 125 The area is located at the farthest peripheries of the more established areas, and many of the residents who are employed are obliged to spend much time travelling by bus or taxi to the more established areas for work, or to seek work. “Khayelitsha has an estimated population of 407 050, and is mainly inhabited by Xhosa speaking people who have moved from rural areas of the Eastern Cape Province. Khayelitsha has among the worst socioeconomic and health indicators in Cape Town; only 36% of adults are employed, 80% of the population live in poor housing conditions, the infant mortality rate is 43 per 1 000 live births, the tuberculosis incidence rate is 978 per 100 000 and the homicide rate is 120 per 100 000.” (Bradley & Puoane, 2007: 50) Community Health Workers march through the township of Khayelitsha to create community awareness in non-communicable diseases and their prevention. Khayelitsha, Cape Town, South Africa, 2005. Community Health Workers (CHWs) working in Khayelitsha and employed by a nongovernmental organization voiced concerns about the increasing problem of hypertension and diabetes in their community area and the poor health services available for managing these conditions. Researchers at the Medical Research Council and the School of Public Health at UWC responded to these concerns by proposing a participatory action research project to SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 126 understand the situation and empower the CHWs to address the problems. The quotations at the beginning of this section are from some of the CHWs in the NGO. Deaths per 100 000 population: Differences between sub-districts in Cape Town, South Africa (Source: Groenewald P, Bradshaw D, Daniels J, Matzopoulos R, Bourne D, Blease D, Zinyakatira N, Naledi NT. Cause of death and premature mortality in Cape Town, 20012006. Cape Town: South African Medical Research Council, 2008.) SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 127 Age standardized mortality rate for broad cause groups by sub-districts, 2006 (Source: Groenewald P., Bradshaw D., Daniels J., Matzopoulos R., Bourne D., Blease D., Zinyakatira N., Naledi N. T. Cause of death and premature mortality in Cape Town, 2001–2006. Cape Town: South African Medical Research Council, 2008.) 3.1 Towards a definition of non-communicable diseases TASK 1 – Define NCDs Part 1 Before you start, jot down four key features of NCDs. Now see if you can find a definition on the WHO site. Part 2 The following terms are often encountered in this context. How do you understand these terms? What do they refer to? Please give at least one examples of each group of disease. Chronic disease: Chronic non-communicable disease: Pre-transitional diseases: SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 128 FEEDBACK Four key features of non-communicable diseases: Non-communicable diseases do not have a single causal agent that must be present for the disease to occur; They are diseases generally caused by multiple factors; There is often a long latent period before the disease becomes evident and it is often incurable; It may lead to disability and last for life (become chronic). The terms “chronic disease” and “non-communicable disease” may sometimes be used almost interchangeably, but they are not strictly the identical. A chronic disease is a disease that, once contracted, will last a lifetime, or a very long time, regardless of causal factors or the risk factors believed to lead to its development. Most chronic diseases are non-communicable, but there are some that are communicable. Chronic disease does not therefore refer merely to a non-communicable disease. For example, HIV/AIDS is a communicable disease with a single causal agent – the HIV. There is currently no known cure for HIV and consequently when someone contracts HIV they will always have HIV. Nowadays, the disease can be controlled with antiretroviral medication, thus allowing the sufferer to lead a very long life not much different to a normal, disease free lifespan; therefore, it is now largely considered to be a chronic disease. The focus of this module is “non-communicable diseases”, denoting those diseases that do not have a single causal factor like a vector, which develop from multiple factors (See section 3.3. below for an extended discussion on how we may understand “cause” and “risk factor”), last for life and may lead to disability or eventually, death. Non-communicable diseases are generally chronic, but not all chronic diseases are communicable. Pre-transitional disease: Lucas & Gilles (2003) speak of “… communicable diseases, malnutrition, and problems associated with pregnancy and childbirth [which] have come under control. When we speak of “pre-transitional diseases”, we are speaking of this group of health issues that contribute to the burden of disease; the predominant diseases / health issues that existed before “… the spectacular shifts in the patterns and causes of death that have taken place in most countries”, as Unit 2 session 2, quoting Beaglehole & Bonita (2001: 6), and which predominated before he epidemiological transition. There is ample evidence showing that non-communicable diseases are increasing in developing countries and that globally, poor and disadvantaged populations are being affected disproportionately. This has the effect of widening health gaps both between and within countries (Gwatkin, 1999). At the same time, within some populations – particularly those in richer countries, the risk of developing NCDs increases as the number of older people in the population increases. In other words, demographic changes affect the increase of NCDs. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 129 Age distribution of burden of disease by income group, 2004 SOURCE: WHO. (2004). Global Burden of Disease 2004 Update: Selected figures and tables. Geneva: WHO. The disproportionate burden on the poor is further illustrated by the two graphs accompanying the Khayelitsha case study above. 3.2 Major non-communicable diseases Five types of non-communicable diseases make the largest contribution to mortality in low and middle income countries. These are the major non-communicable diseases categories - cardiovascular disease, diabetes and cancer. Within these categories, there are differences in prevalence between the sexes. They are: cardiovascular disease diabetes chronic lung diseases cancer mental health disorders (depression At this stage, you should revise the concepts of the Demographic and Epidemiological Transitions in your setwork – Short Textbook of Public Health Medicine for the Tropics. Study Chapter 8 from Lucas & Gilles (2003), pages 235-236. Key to addressing NCDs is understanding the nature of each disease and its risk factors. Although you have probably used the concept before, here is some clarification of what is meant by risk factor in the scientific context. In brief, a risk factor is an exposure (to a factor) which is associated with a disease. This phrase associated with is important: association between factors suggests that there is a linkage between the SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 130 factors. However, Friis & Sellers (2004: 69) point out: “Because of the uncertainty of causal factors in epidemiological research, it is customary to refer to an exposure that is associated with a disease as a [risk factor].” There are three requisite criteria for something to be considered a risk factor (Friis & Sellers, 2004). When can something be called a risk factor? 1. The frequency of the disease varies by category or value of the factor. This means that light smokers are more likely to develop lung cancer than nonsmokers and heavy smokers are more likely to develop it than light smokers. 2. The risk factor must precede the onset of disease. If we want to say that smoking is a risk factor for lung cancer, then individuals must have started smoking before they get lung cancer. 3. The observed association must not be due to a source of error. This takes into account the selection, measurement and analysis procedures and will be covered in more detail in your Descriptive Epidemiology module. It has been estimated that up to 80% of cardiovascular disease and diabetes and over a third of cancers could be prevented if these risk factors were eliminated. Interestingly, the first four diseases listed at the beginning of this section share similar risk factors and intervention strategies. On the other hand, mental health disorders share one of the risk factors, alcohol misuse, but other risk factors and the preventive and management strategies are different. While “risk factor” may not be translated as “cause” – because of the difficulties mentioned above, there has been a substantial number of research studies associating certain risk factors with the onset of particular non-communicable diseases, enough to substantially convince many Public Health practitioners and researchers that addressing the risk factors should have a demonstrable effect on the incidence and prevalence of the associated disease condition. Now explore the nature of these five main NCDs and try to locate their risk factors in the literature or on the internet. TASK 2 – Familiarize yourself with NCDs 1. Read about the different NCDs and search for their risk factors: use the WHO website, other internet sites or a textbook and write them into the right hand column in pencil; then connect al the diseases with the risk factors using lines. In the process, look for common risk factors, or factors which are associated with the onset of the disease. 2. Look back at the top 20 causes of mortality and DALYS for your country (developed in Session 2). Identify major risk factors of each of the non-communicable diseases. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 131 DISEASE DESCRIPTION NCDs The major diseases in this category include hypertensive disease, stroke and ischaemic heart disease, as well as pretransitional diseases, such as rheumatic heart disease. 1. Cardiovascular Disease RISK FACTORS (SA info). Diabetes is a metabolic disorder resulting in an elevated blood glucose which occurs when the pancreas does not produce enough insulin, or the body cannot effectively use the insulin it produces. Diabetes is classified into three groups: Type 1, Type 2 and Gestational Diabetes. Type 2 contributes 90% of diabetes burden globally. 2. Diabetes The main chronic respiratory diseases include chronic obstructive pulmonary disease (COPD), asthma, occupational lung diseases, and lung cancer. 3. Chronic lung Disease (SA info). SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 132 Neoplasms, tumors are growths that arise from normal tissues. They may be benign (not problematic) or malignant (dangerous and life threatening). Cancers may occur at any age but are more common in the elderly. They are associated with exposure to specific carcinogens, like cigarette smoking, but in many cases causative substances have not been identified. 4. Cancer (Neoplasms) The leading causes of death vary with cancer of the lung, breast, colon and prostrate gland common in developed countries, and cancer of the cervix, oesophagus and liver common in developing countries. Recent data from South Africa indicates the following top causes of cancer deaths Men: lung, Kaposi’s sarcoma, oesophageal cancer. Women: cervix, breast and Kaposi’s sarcoma. Sitas, Parkin, Chirenje, Stein, Abratt & Wabinga (2008), cited in Mayosi, Fisher, Lallo, Sitas, Tollman & Bradshaw (2009: 60) SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 133 Mental disorders include depression, alcohol-use and substance-use disorders, schizophrenia and dementia. There is an Increasing awareness of mental disorders as a significant cause of morbidity. 5. Mental Health Disorders (Depression)/Neuropsychiatric Disorders When health problems were ranked using mortality rates, the importance of mental disorders was underestimated, but now that the measurement of burden of disease includes a calculation of disability there is a greater appreciation of mental disorders as an important component of the burden of disease in any specific context. Mental disorders are related to other health problems in that mental disorders can increase the risk for other diseases, and in a similar manner other diseases can increase the risk for mental disorders. Other non-communicable diseases of public health importance include osteoporosis, renal diseases, oral diseases, genetic diseases, neurological diseases and diseases causing blindness and deafness. 6. Other noncommunicable diseases SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 134 Risk factors are divided into non-modifiable and modifiable risk factors. Non-modifiable risk factors are those that cannot be changed such as biological factors, age, sex; hereditary factors, and early life experiences, e.g. catch-up growth or stunting, excessive body weight, hypertension, Modifiable risk factors are those behaviours that can be altered such as physical inactivity, poor nutrition, tobacco use, excess alcohol use. Social determinants of health underpin many of the causes of NCDs and include urbanisation and globalisation resulting in dietary changes, adoption of unhealthy behaviours, e.g. smoking; environmental factors such as poor food choices, reduced physical activity, and an obesogenic environment which promotes poor food choices, barriers to physical activity, e.g. lack of recreational facilities, unsafe walking environments as well as cultural beliefs about body weight. Some NCDs are to some extent preventable and share a number of common risk factors (as you will have noticed in your table in TASK 2). These risk factors accumulate throughout the life course. Tackling shared modifiable risk factors can be an effective strategy, because, by addressing them, they feed into reducing several NCDs at the same time. For example, tobacco use, physical inactivity unhealthy diets and harmful use of alcohol are all behavioural risk factors for several NCDs. Risk factors for NCDs can be located in a wider context as well - arising from a set of underlying environmental determinants which can be broken down into social (e.g. cultural), economic, physical and political. The underlying determinants must also be addressed to effect change on NCDs: “Chopra and Puoane, in a study to identify environmental risk factors for non-communicable diseases in an urban township, found that there was generally a shortage of healthy, low-fat food, and little fresh fruit and vegetables available in the townships. The majority of shops sold cheap fatty foods and stalls run by street vendors often sold fatty meat and sausages” (Puoane, Tsolekile, Sanders & Parker, 2008:79). You will remember that the WHO Commission on Social Determinants of Health focused attention on social and economic factors which affect health: this includes the effects of poor living environments, social exclusion and economic deprivation on health. Although evidence is not conclusive there is a growing perception that poverty and its underlying factors have a significant impact on non-communicable diseases. Beaglehole and Yach (2003) draw our attention to the direct and indirect effects of globalization on promoting the risk factors for non-communicable diseases – for example, advertising and marketing of certain fast foods has created an obesogenic SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 135 environment (one which promotes obesity) where these foods are socially desirable especially amongst young people; furthermore they point to the way in which tobacco, alcohol and nutrition legislation have indirect effects on national economies and health systems. One of the key current understandings on NCDs is that biological, behavioural and structural (which takes into account the lessons of the social determinants framework) factors are implicated in the development – incidence and development over their course – of this category of disease. Tackling NCDs, therefore, generally requires integrated action on risk factors and determinants across sectors, coupled with strengthening health systems to improve prevention and control. On the other hand, health professionals need to be mindful that community members cannot always control the behavioural determinants even though they are apparently modifiable. To reinforce this point, we have avoided using the term “Chronic diseases of lifestyle” or CDLs – as this group of diseases has been known for sometime previously – for these NCDs. The term suggests that all that is required is a change of lifestyle, and these diseases can be avoided; it appears however, that individuals’ and community circumstances might not make this possible. TASK 3 – Consider the burden of NCDs Read the case study above of Khayelitsha under section 3 and answer these questions: 1. Why do you think non-communicable diseases are increasing in Khayelitsha? 2. Try to find statistics relating to NCDs in your country or region. Which diseases are most prevalent? Save these statistics as you will be using them in the Discussion Forum. FEEDBACK Some of the factors which are thought to be fuelling the growth of NCDs The overall social, economic and environmental situation has a huge impact on individual lives. This tends to reduce individual choice. Specifically: Changes in diet and physical activity due to living environment Urban, rather than rural (in general, less physical activity as no longer engage in intense physical activity required to produce food, shorter travel distances, greater availability of transport) High unemployment – not much money available to buy healthy foodstuffs, which tend to be more expensive on the national economic market Limited choice in food sources SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 136 TASK 4 – To what extent are NCDs preventable? Take a look at this cartoon: Mrs Mashishi has presented to the doctor with symptoms of an NCD. 1. Consider why this doctor’s response could be called victim-blaming. 2. Then formulate what you could rather say to Mrs Mashishi and what you would recommend to the district health manager in relation to women in this community like Mrs Mashishi. Well, Mrs Mashishi, you simply have to take better care of yourself – more exercise, less fatty foods, and above all, less stress. Mrs Mashishi is a mother of four young children; her husband is unemployed, and drinks heavily over weekends. She works as a factory cleaner. Where she works, there are a few small cafes mostly selling junk food. She moved to Cape Town after the birth of her second child five years ago. She works from 08h00-17h00 daily and reaches home at 18h30. She hopes one day to build a block house but lives in a shack presently. FEEDBACK In your response, did you consider what non-modifiable factors could be at play in this situation? And while stress is a risk factor for hypertension, what success rate would you give the chance of Mrs Mashishi being able to reduce her stress? In previous years, many of the popular models of dealing with NCDs emphasized the personal factors, and the concept of personal control in modifying one’s risk and SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 137 reducing one’s chances of losing life years to disease. Subsequently, many studies have shown that there is more to the acquisition & maintenance of health than the personal factors. The increasing importance of the idea of social determinants acknowledges this. In the following section, we will outline a few of the recommendations on the factors to consider if wishing to make an impact in reducing the burden of non-communicable diseases. The reading accompanying the section makes various important points. 4 RESPONDING TO THE CALLENGES OF NCDs The implications of NCDs increasing unabated are serious at many levels: they have economic impact at individual, household, social and national levels, e.g. through the cost of treatment and medication to the state, loss of earnings to the individual and family, and loss of productive labour to the nation, and reduced quality of life for the individual. Treating chronic diseases also puts substantial economic and human resources strain on health systems (Puoane, Tsolekile, Sanders & Parker, 2008). The Final Report of the WHO’s Commission on Social Determinants (2008) makes the point forcefully in the following diagram illustrating the WHO’s working framework on social determinants. As you’ve established in Unit 1, session 1, the social determinants framework provides a useful tool both for tracking the development of health conditions and for working towards addressing the health conditions. Additionally, the shift from acute care to chronic care also places substantial demands on health services and has human resources cost implications. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 138 In the SOPH module Population Health and Development: A Primary Health Care Approach I, four key pillars of population health were identified: promotion, prevention, curative and rehabilitative. This, together with an increasing body of evidence, suggests some key points of action: Policy development and implementation. Promotion of healthy living lessons and advocacy Detection (of disease in potentially affected populations) Measurement – ongoing measurements of disease incidence and / or progression indicators in the (potentially affected) population, as well as the capacity to do so. Pharmacological control Behaviour change (also often referred to as “lifestyle”) change Monitoring of the actions as well as health indicators in the population of concern 4.1 The global response It is widely recognized that tackling NCDs needs integrated action on risk factors and their determinants across sectors, as well as consistent strengthening of health systems to improve prevention and control. The WHO’s recently launched 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases outlines strategies “to establish and strengthen initiatives for the surveillance, prevention and management of NCDs” (WHO, 2008:5). This initiative is built on the previous Global Strategy endorsed in 2000 which had: 1. To map the emerging epidemics of non-communicable diseases and analyse their social, economic, behavioural and political determinants. 2. To reduce the level of exposure of individuals and populations to the common risk factors for non-communicable diseases and their determinants. 3. To strengthen health care for people with non-communicable diseases. It also built on other global initiatives listed in the table below, and is intended to guide national and regional strategies and action plans. The action plan set out six objectives to implemented over the six-year period 2008-2013. Objective 1: Objective 2: Objective 3: Objective 4: Objective 5: Objective 6: To raise the priority accorded to non-communicable disease in development work at global and national levels, and to integrate prevention and control of such diseases into policies across all government departments. To establish and strengthen national policies and plans for the prevention and control of non-communicable diseases. To promote interventions to reduce the main modifiable risk factors for non-communicable diseases: tobacco use, unhealthy diets, physical inactivity and harmful use of alcohol. To promote research for the prevention and control of noncommunicable diseases. To promote partnerships for the prevention and control of noncommunicable diseases. To monitor non-communicable diseases and their determinants and evaluate progress at the national, regional and global levels. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 139 The global response to address non-communicable diseases DATE 2000 2003 2004 2007 2008 2008-2013 STRATEGY Global Strategy for the Prevention and Control of Non-communicable Diseases WEBSITE http://www.who.int/ncd/mip2000/do cuments/wha_53_17_en.pdf WHO Framework Convention on Tobacco Control http://www.who.int/tobacco/framew ork/WHO_FCTC_english.pdf Global Strategy on Diet, Physical Activity and Health http://www.who.int/dietphysicalactiv ity/strategy/eb11344/strategy_engli sh_web.pdf Resolution WHA60.23 on Prevention and control of noncommunicable disease: implementation of the global strategy WHO Report on the Global Tobacco Epidemic, 2008 – The MPOWER Package Resolution WHA61.4 on Strategies to reduce the harmful use of alcohol http://apps.who.int/gb/ebwha/pdf_fil es/WHA60/A60_R23-en.pdf http://www.who.int/tobacco/mpowe r/mpower_report_full_2008.pdf http://www.who.int/substance_abus e/activities/4ai.pdf Medium-term Strategic Plan 2008– 2013 http://whqlibdoc.who.int/hq/2007/M TSP08-13_PB08-09_cor1_eng.pdf Action Plan for the Global Strategy for the Prevention and Control of Non-communicable Diseases http://whqlibdoc.who.int/publication s/2009/9789241597418_eng.pdf (Adapted from WHO, 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Non-communicable Diseases.) 4.2 National-level Policy Initiatives Subsequent to the launch of the WHO initiatives, many countries have developed their own national policies or guidelines to address risk factors for non-communicable (a photographically similar document saved in portable document format).e diseases. TASK 5 – Relate the global strategy to your own context 1. Skim-read the 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Non-communicable Diseases document which can be accessed online at http://www.who.int/nmh/Actionplan-PC-NCD-2008.pdf. Take note of the six objectives, and the national level implications proposed action by Member States. 2. Identify any policies which are in place in your country to address noncommunicable diseases. 3. Identify any actions which seem viable for your country to address. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 140 FEEDBACK As an example of a national-level policy initiative, South Africa has introduced a number of key policies and guidelines to address non-communicable diseases: 1. 2. 3. 4. The Tobacco Control Act (Act 83 0f 1993) was amended in 1999 and 2007. The Liquor Act (Act 59 of 2003). Food-based dietary guidelines developed in 2001. National guideline for the management and control of non-communicable diseases published in 2006. 5. Vuka South Africa – Move for Health Initiative launched in 2005. 6. Mental Health Care Act (2002). 4.3 The Role of Primary Health Services Chronic non-communicable diseases need ongoing monitoring and management, rather than the once off treatment suitable for acute conditions and so different systems need to be put in place for this, as most primary level services in developing countries are geared towards acute conditions. “Successful prevention and management of chronic non-communicable diseases is dependent on an effective health service approach, as well as on the approaches of health promotion and primary prevention” (Puoane, Tsolekile, Sanders & Parker, 2008: 81 citing Charlton, Brewitt & Bourne, 2008). In considering a response to managing NCDs, read these two articles. READINGS Beaglehole, R., Epping-Jordan, J., Patel, V., Chopra, M., Ebrahim, S., Kidd, M. & Haines, A. (2008). Improving Prevention and Management of Chronic Disease in Low-income and Middle-income Countries: A Priority for Primary Health Care. Lancet, 372: 940–949. Puoane, T., Tsolekile, L., Sanders, D. & Parker, W. (2008). Chronic non-communicable diseases. South African Health Review. Durban: Health Systems Trust: 73–87. Also available [Online]: http://hst.org.za/uploads/files/cont_ack_08.pdf Downloaded: 03 / 12/09 TASK 6: Questions to focus your reading of the article As you read the article focus your mind with questions in order to note the key points. Questions to bear in mind while you read 1. Key ways in which the primary health care system needs to change in order to cope with the increasing burden of non-communicable disease: How do health systems need to change to respond to the management of CDs? How do health systems need to change from a (predominantly) acute, curative approach to a form more suitable for the management of NCDs? SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 141 2. How do health systems need to change to: Have an integrated approach to prevention and management Focus on a monitoring approach Focus on, and build, health teams to work together in the management of NCDs Focus on building self-management skills and capacity among individuals. 3. What other types of strategies or interventions were mentioned in the readings? 4. Keeping your working context in mind, how do you rate the chances of the strategies discussed above to be successfully implemented? FEEDBACK We trust that the framework developed in this section will provide insights into the effective prevention and management of NCDs in any setting from the global to the local. Local may range from national to the community level; the input on Community Health Workers and their potential for an impact on the burden of non-communicable diseases – briefly looked at in the Khayelitsha case study at the beginning of this study session and more comprehensively (with a Reading) in the SOPH module Population Health and Development: A Primary Health Care Approach I. In addition, it has been recently acknowledged that primary health systems are critical in delivering mental health services and WHO have identified the need for building community-based mental health systems and services. A number of key components for improving mental health services have been identified and these include: provision of treatment for mental disorders at primary care level; ensuring increased accessibility to essential psychotropic medication, and providing care in the community; educating the public; involving communities, families and consumers. The importance of actively involving communities in preventive and control strategies is also recognized focusing on risk reduction, community mobilization and participation. A number of small scale projects have been initiated but have yet to be taken up to scale. TASK 7 – Exploring NCDs in your own setting ◙This task is important because it forms the basis of the Discussion Forum topic in preparation for your assignment. 1. Prepare a short profile of your district or sub-district as regards NCDs. In this description, discuss: where it is situated; relevant climatic and geographical features; demographic and economic features; population size and health facilities; 2. Find any available statistics on the NCD status of the population of the country, or the district. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 142 3. Find out how are primary level services are catering for people with chronic noncommunicable diseases. 4. Are there any local community-based initiatives in your district or country to address non-communicable diseases? FEEDBACK You are expected to present your country profile to your fellow students, and to discuss them critically. You will work together to identify relevant initiatives, missed opportunities and potential challenges for your district. 5 SESSION SUMMARY Current evidence points to an increasing burden of non-communicable diseases in the developing world. Prevention and management of non-communicable diseases in resource constrained countries are challenging and will require innovative strategies to address the situation. In summary, Mayosi, Flisher, Lallo, Sitas, Tollman, & Bradshaw (2009: 64) list a series of recommendations which they have developed for the country of South Africa which, as a “developing country”, is nonetheless characterized by its own particular socioeconomic conditions and health indicators. Panel 2: Recommendations of priority population-level interventions to the national Department of Health for the prevention of chronic diseases in South Africa 1 Maintain and extend tobacco-control activities, especially for young people, and encourage quitting by means of counselling and nicotine replacement therapy. 2 Monitoring, assessment, and enforcement of occupational health and antialcohol legislation. 3 Food-control legislation with public education for reducing the salt content of food and for substituting 2% of trans fat with polyunsaturated fat. 4 Promotion of physical activity in schools, workplaces, and the built environment. 5 Electrification of households to reduce exposure to biomass pollutants and reduce the burden of COPD*. 6 Prevention and control of tuberculosis through enhanced notification and contact tracing to reduce the burden of COPD*. 7 Use of multidrug regimes (e.g. the polypill containing asprin, β blocker, ACE inhibitor, diuretic, and a statin), and an absolute risk approach to prevent stroke, chronic kidney disease, hypertensive heart disease, and ischaemic heart disease. 8 Assess the cost-effectiveness of rolling out the HPV 16/18 vaccination in view of emerging cheaper HPV screening technologies. 9 Strengthen the district-based primary health system, with sites of service excellence, and integration of the care of chronic diseases and their risk factors. 10 Develop a national surveillance system for all chronic diseases. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 143 *COPD-chronic obstructive pulmonary disease ACE-angiotensin converting enzyme HPVhuman papillomavirus. SOURCE: Mayosi, Flisher, Lallo, Sitas, Tollman, & Bradshaw. (2009). The burden of noncommunicable diseases in South Africa. The Lancet, Health in South Africa: 64 Given that these recommendations address generally established risk factors of NCDs in relation to a single and particular country, is there anything that you can take from this list to apply in your own work context. Reflect on how these risk factors could impact on global or national health systems and also how they relate to a single unique work environment? 6 REFERENCES AND FURTHER READING (Beaglehole R. & Yach D. (2003). Globalisation and the prevention and control of non-communicable disease: the neglected chronic diseases of adults Lancet: 362; 903-908). A Global framework for action to improve the primary care response to chronic noncommunicable diseases Maher Beaglehole R. & Yach D. (2003). Globalisation and the prevention and control of non-communicable disease: the neglected chronic diseases of adults Lancet: 362; 903-908 Beaglehole, R. & Yach, D. (2003). Globalisation and the Prevention and Control of Non-communicable Disease: the Neglected Chronic Diseases of Adults Lancet: 362; 903-908 Bradley H, Puoane T. (2007). Prevention of hypertension and diabetes in an urban setting in South Africa: Participatory action research with community health workers. Ethnicity & Disease 17: 49-54. Commission on Social Determinants of Health. (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organisation. CSDH. (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization. Gwatkin, D. R., Guillot, M. & Heuveline, P. (1999). The burden of disease among the global poor. Lancet:: 154 (9178): 586-589. Mayosi, B. M., Flisher, A. J., Lallo, U. G., Sitas, F., Tollman, S. M. & Bradshaw, D. (2009). The burden of non-communicable diseases in South Africa. The Lancet: Health in South Africa. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 144 Mayosi, B. M., Fisher, A. J., Lalloo, U. G. et al. (2009) The burden of noncommunicable diseases in South Africa. Lancet: 1581. MDGs: chronic disease are not on the agenda Lancet 366 1512-1514 Non-communicable disease must be given greater priority, says WHO. BMJ 2009: 339: 130-131. Strong, K. Preventing chronic disease: how many lives can we save? Prince, M., Patel, V., Saxena, S., et al. (2007). No health without mental health. Lancet: 370: 859-877. Puoane, T.,Tsolekile, L., Sanders, D. & Parker, W. (2008). Chronic NonCommunicable Diseases. South African Health Review. Durban: Health Systems Trust: 73 – 87. Also available from: [Online], Available: http://www.hst.org.za. Sengwana, M. J., Puoane T. (2004). Knowledge, beliefs and attitudes of community helath workers about hypertension in the Cape Peninsula, South Africa. Curationis. 27 (1) 65-71 Strong, C., Mathers, S., Leeder, Beaglehole, R. (2005) Quote from: Preventing chronic diseases: how many lives can we save? K Lancet 2005; 366: 1578–1582. The burden and costs of chronic diseases in low-income and middle-income countries Abegunde DO The neglected epidemic of chronic disease. Lancet 366: 1514 WHO. 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Non-communicable Diseases WHO. (2008). Global Strategy for the Prevention and Control of Non-communicable Diseases: Action Plan, 2008-2013. Geneva: WHO. [Online], Available: http://whqlibdoc.who.int/publications/2009/9789241597418_eng.pdf SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 145 SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 146 Unit 2 – Session 5 Injuries and Violence Introduction In the final session of this unit we will focus on injuries and violence - the third group of causes of death in the global BOD study. In this session we will define injuries and violence, look at the burden caused by injuries and violence, and at sources of information. We will follow this by looking at risk factors for unintentional injuries and violence and then finally we will focus on current preventive strategies. In recent years, the WHO have increased their activities in the field of injuries and violence prevention with a number of key reports. The names and links to key reports are included as additional resources at the end of this session. Injuries and violence are important causes of death and disability globally. The 2005 WHO Report estimated that 5.4 million deaths from injury accounted for 9% of all deaths worldwide and 12% of the global burden of disease. Injuries primarily affect young adults with eight of the 15 leading causes of death for people between the ages of 15 and 29 years being injury-related. These include road traffic accidents, suicides, homicides, drowning, burns, war injuries, poisonings and falls. The extent of non-fatal injuries varies from country to country but for every death it is estimated that there are many hospitalisations and visits to accident and emergency departments. A large proportion of people surviving their injuries incur temporary or permanent disabilities. Whilst violence and injuries occur in all countries, they are unevenly distributed and are generally higher in low- and middle-income groups, where unsafe living, working and travelling conditions are more common. In these areas there is often a lack of prevention measures or treatment and rehabilitation facilities are inadequate. “In some parts of the world, the public health community has long recognized injuries as a major public health problem. In other countries, the enormous medical, social and economic costs of violence and injuries are only now being recognized and serious efforts begun to prevent injuries and address their consequences”. (World Health Organisation. Preventing Injuries and Violence: A Guide for Ministries of Health. Geneva: WHO, 2007: 5) Injuries and violence are sometimes perceived as an inevitable part of life and in general the health sector has responded in a largely reactive and therapeutic manner. It has been recognised more recently, however, that injuries and violence are complex phenomena and need to be addressed in a comprehensive way. A Public Health approach which focuses on the health of populations and communities, has a promotive and preventive focus. It is multidisciplinary, promoting partnerships with other sectors more likely to yield positive results in the prevention of injuries and violence. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 147 The Public Health approach to injuries and violence is illustrated in the figure below. Figure 1: Public Health approach to injuries and violence (Source: World Health Organisation. Preventing Injuries and Violence: A Guide for Ministries of Health. Geneva: WHO, 2007: 23 www.who.int/violence_injury_prevention/publications/injury_policy_planning/prevention_moh/en/) As you are working through this session, think about why injuries and violence should be the concern of Public Health. We will come back to this question later in the session. DEFINITION OF INJURIES “Injuries were traditionally defined as physical damage to a person by acute transfer of energy (mechanical, thermal, electrical, chemical or radiation) or by sudden absence of heat or oxygen” (REF International Public Health (Big Book), 323). However this definition has now been broadened to include psychological harm and deprivation. Injuries are commonly categorised into unintentional and intentional injuries. Unintentional injuries include injuries sustained as the result of road traffic accidents, poisonings, falls, burns and drowning, as well as occupational injuries and sports injuries. Intentional injuries or violence are injuries where there is evidence that the injury was planned. However recently injuries where there is an intention to use force or violence, but not necessarily an intention to injure, have been included in this definition. Contents 1 2 3 4 5 6 7 Learning outcomes of this session Readings Data on injuries and violence Intentional and unintentional injuries Session summary Useful resources Reference SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 148 1 LEARNING OUTCOMES OF THIS SESSION By the end of this unit you should be able to: Demonstrate an understanding of key concepts in relation to injuries and violence. Demonstrate an understanding of injuries and violence and their risk factors. Demonstrate an understanding of the range and interaction of factors on injuries and violence. Demonstrate familiarity with scholarly sources of information on injuries and violence. Demonstrate familiarity with prevention interventions for injuries and violence. 2 READINGS The readings for this session are listed below. You will be directed to them in the course of the session. Author/s Publication details Krug, E. G., Mercy, J. A., Dahlberg, L. L. & Zwi, A. B. Norton, R., Hyder, A. A. & Gururaj, G. (2002, October 5). The World Health Report on Violence and Health. Lancet 360: 1083-1088. (2008). Ch 7 - Unintentional Injuries and Violence. In M.H. Merson, R.E. Black & A.J. Mills (eds). International Public Health. Jones and Bartlett Publishers: 330-347. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 149 3 DATA ON INJURIES AND VIOLENCE TASK 1 - Identify sources of data 1. Think of, and write down, some sources where you will be able to access data on violence and injuries. Data on injuries and violence can be obtained from within and outside the health sector. FEEDBACK HEALTH SECTOR Health Information Systems Vital registrations Hospital data Ambulance records Trauma records OTHER SECTORS Police records Transport records Legal records Insurance companies In addition, other sources may be available for specific types of injuries, for example – Road Traffic Accidents. In general, better data is available for deaths from injuries and violence as opposed to morbidity and disability. Data from middle- and low-income countries, including subSaharan Africa is often poor, however in the past few years South Africa (SA) has made concerted efforts to gather information on deaths due to injuries. National Injury Mortality Surveillance System (NIMSS) In SA, the Department of Health commissioned the Medical Research Council (MRC) to develop a National Injury Mortality Surveillance System (NIMSS). This system collects information on all deaths from unnatural causes from mortuaries across the country and it is used with the vial registration data (death certificates) for compiling statistics on injury mortalities which can be used for planning and monitoring purposes. For further information see: www.sahealthinfo.org/violence/nimss.htm SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 150 Figure 1: The high burden of injuries in South Africa Source: Norman R, Bradshaw D, Schneider M, Pieterse D, Groenewald P. Revised burden of disease estimates for the comparative risk factor assessment, South Africa 2000. Methodological notes. Cape Town: South African Medical Research Council; 2006. Available at: http://www.mrc.ac.za/bod/reports.htm.Rosana Norman a, Richard Matzopulos b, Pam Groenewald a, Debbie Bradshaw a Of the estimated 59 935 injury deaths in 2000, 46% (27 563) were homicides. Road traffic and self-inflicted injuries accounted for 26.7% and 9.1% of the injury mortality, respectively. Homicide was the leading cause of fatal injury in males; road traffic injuries ranked second. This order was reversed in females. In South Africa injury and violence are the second leading cause of death and disability. In 2000 the overall death injury rate was 157 per 100 000 which is twice the global average, and the rate of homicide by intimate partners is six times the global average. TASK 2 - Identify common causes of injury mortality 1. What are the main causes of injuries in your country? Compare them to the global and SA burden. 2. How is information on injuries complied in your country? What data sources are used? 3. What could be done to improve the data further and whose role is this? SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 151 4 INTENTIONAL AND UNINTENTIONAL INJURIES Unintentional injuries The first group of injuries we will look at are unintentional injuries. The leading causes of unintentional injuries are: Road traffic accidents Falls Burns Poisoning Drowning Risk factors for unintentional injuries The body of research and evidence on risk factors for injuries is increasing and although much of the work comes from high-income countries – there is increasing amounts of work from middle- and low-income countries. READING Norton, R., Hyder, A. A. & Gururaj, G. (2008). Ch 7- Unintentional Injuries and Violence. In M.H. Merson, R.E. Black & A.J. Mills (eds). International Public Health. Jones and Bartlett Publishers: 330-335 Read the above pages and then jot down in the table below some of the main risk factors for the most common unintentional injuries that apply in your country. Do this by listing the main age-group and the settings at risk. Table 1: Unintentional injuries and risk factors UNINTENTIONAL INJURY Road traffic accidents AGE GROUP AT RISK MAIN SETTINGS Falls Poisonings Burns Downing SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 152 Intentional injuries (violence) The second group of injuries is unintentional injuries or violence. Violence has been defined in the following way. Violence: “The intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community, that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment or deprivation”. (WHO, 1996) Violence is a complex concept and frameworks have been developed to highlight the common features and linkages between different types of violence. The first World Report on Violence and Health in 2002 categorised violence into three broad categories according to who commits the violent act and then further divides these categories into specific types of violence. READING Krug, E. G., Mercy, J. A., Dahlberg, L. L. & Zwi, A. B. (2002). The World Health Report on Violence and Health. Lancet; 360: 1084 Read Figure 1 on page 1084. The three categories from the World Health Report on Violence and Health are: Self-directed violence: This includes suicidal behaviour and self-abuse such as selfmutilation. Interpersonal violence: This is divided into two sub-categories: Family and intimate partner violence which includes: child abuse, intimate partner violence and abuse of elderly. Community violence which includes: youth violence, sexual violence by strangers, and violence in institutional settings. Collective violence: This is the use of violence by people who identify themselves as members of a group against another group, in order to gain political, economic or societal objectives. This includes armed conflicts, gangs and organised violent crime. Risk factors or roots of violence As we have already stated, violence is complex and cannot be attributed to one cause, but has its roots in the interaction of many factors – biological, social, cultural, economic and political. The World Health Report on Violence and Health uses an ecological model with four levels to represent the complexity. First level: Individual – biological and personal factors that influence how people behave. Second level: Close relationships, such as those with family and friends. In youth violence, having friends who engage in violence is a risk and for intimate partner violence, marital conflict is important. Third level: Community context – neighbourhood, schools, workplaces are important. Fourth level: Societal factors such as social and cultural norms, income inequality, social welfare and justice systems, availability of firearms and political instability. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 153 The model illustrates the interaction of factors at the different levels and suggests that in order to prevent violence it is necessary to act across the different levels at the same time. Injury and violence prevention “Prevention concentrates upon identifying ways to keep people from committing acts of violence and of stopping the events that lead to unintentional injuries from occurring. It is achieved by removing or reducing the underlying causes and risk factors. Effective prevention saves lives, reduces disabilities and other health consequences, and is increasingly being shown to be cost effective”. (World Health Organisation. Preventing Injuries and Violence: A Guide for Ministries of Health. Geneva: WHO, 2007: 22) TASK 3 – Identify reasons why injuries and violence should be the concern of Public Health Read pages 17–20 of the reading, your setwork for Descriptive Epidemiology and then answer the questions below. READING Norton R, Hyder A. A. & Gururaj G. (2008). Ch 7- Unintentional Injuries and Violence. In M.H. Merson, R.E. Black & A.J. Mills (eds). International Public Health. Jones and Bartlett Publishers: 345-347 1. Going back to the question we posed near the beginning of this session: Why should injuries and violence be the concern of Public Health? In order to answer this question, bear in mind what you have already learnt about injuries and imagination on this one. FEEDBACK Research has provided clear evidence that certain interventions can prevent injuries and violence. However, given the complexity of causality, prevention requires action across a range of sectors at local and national levels. Health, and especially Public Health should play a central role, but other sectors also need to be involved. Public Health can contribute by: Describing the problem Developing solutions Implementing programmes Monitoring and evaluating interventions. Violence and injury prevention interventions Now let’s go back to the Krug reading again and look more closely at tackling violence prevention. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 154 TASK 4 – Identify violence prevention strategies READING Krug E. G., Mercy J. A., Dahlberg, L. L. & Zwi A. B. The World Health Report on Violence and Health. Lancet 2002; 360: 1085-1086 1. Reread the above pages. In what ways does the ‘ecological model’ assist in the development of violence prevention strategies? 2. Gives three examples of how understanding the major types of violence can assist you in developing violence prevention suitable approaches? FEEDBACK The ecological model highlights the importance of developing violence prevention strategies that work at different “levels”, that is, individual, family, community and society. Examples of violence prevention strategies within the family, with a strong evidence-base for effectiveness are: Seat-belts, helmets and enforced blood alcohol limits to prevent Road Traffic Accidents (RTAs) Child-resistant containers to prevent poisonings The recently published WHO Preventing Injuries and Violence: A guide for ministries of health suggested that ministries of health need to address a number of key areas in order to promote injury prevention. These include: Policy making; data collection; services for victims; prevention; capacity building; advocacy. Table 2 below, taken from this report, lists selected violence and injury prevention interventions by cause, effectiveness and health sector role. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 155 SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 156 SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 157 (Source: World Health Organisation. Preventing Injuries and Violence: A Guide for Ministries of Health. Geneva: WHO, 2007. www.who.int/violence_injury_prevention/publications/injury_policy_planning/prevention_moh/en/) SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 158 TASK 5: Analyse injuries and violence in your own country 1. Choose a specific type of injury or violence that causes high mortality in your own country. (Use official data sources to make your selection, if available.) 2. List the risk factors for the injury. 3. State what steps have been taken to reduce the burden of this injury in your country? 4. What else do you think should be done to address this problem further? 5 SESSION SUMMARY This session has focused on key concepts in relation to injuries and violence, including the risk facts. We have discussed the range and interaction of factors on injuries and violence, as well as some prevention interventions. Below is a set of useful resources that may be useful for your own further learning or as a tool to train others. 6 USEFUL RESOURCES TEACH-VIP E-learning is a self-paced curriculum developed by WHO and Education Development Center. The course consists of 20 lessons of approximately one hour in duration covers issues related to unintentional injuries and violence and strategies to address these problems. Click on the link to take you to the site where you can find out more. http://teach-vip.edc.org/ Another useful tool available from the WHO website is a powerpoint presentation: 10 facts on injuries and violence. http://www.who.int/features/factfiles/injuries/facts/en/index.html WHO has produced FACT SHEETS on various topics, check the WHO website http://who.int/violence_injury_prevention Capacity building for preventing injuries and violence: Strategic plan 2009-2013. Geneva: World Health Organisation, 2009. http://www.who.int/violence_injury_prevention/capacitybuilding/strategic_plan/en/in dex.html Developing policies to prevent injuries and violence for policy-makers and planners. Geneva: World Health Organisation, 2005. http://www.who.int/violence_injury_prevention/policy?project?en?index.htmil Krug, E. G., Dahlberg, L. L., Mercy, J. A., Zwi, A. B., Lozano, R., eds. World health report on violence and health. Geneva: World Health Organisation, 2002. http://www.who.int/violence_injury_prevention/violence/world_report/en/index.html Peden, M., Oyegbite, K., Ozanne-Smith, J., Hyder, A. A., Branche, C., Rahman A. K. M. F., Rivara, F., Bartolomeos, K., eds. World report on child injury prevention. Geneva: World Health Organisation, 2008. SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 159 http://www.who.int/violence_injury_prevention/child/injury/world_report/en/index.ht ml Peden, M. M. et al eds. World health report on road traffic injury prevention. Geneva: World Health Organisation, 2004. http://www.who.int/violence_injury_prevention/publications/road_traffic/world_report /en/index.html Peden, M., McGee, K., Sharma, G. The injury chart book: a graphical overview of the global burden of injuries. Geneva: World Health Organisation, 2002. Preventing Injuries and Violence: A Guide for Ministries of Health. Geneva: World Health Organisation, 2007. www.who.int/violence_injury_prevention/publications/injury_policy_planning/preven tion_moh/en/ Norman, R., Matzopoulos, R., Groenewald, P., Bradshaw, D. The high burden of injuries in South Africa. Bull World Health Organ 2007.85: 695-702. Van Niekerk, A., Suffla, S., Seedat, M., eds. Crime, violence and prevention in South Africa: data to action. Tygerberg: MRC: UNISA Crime, Violence and Injury Lead Programme, 2008. 7 REFERENCES Krug, E. G., Dahlberg, L. L., Mercy, J. A., Zwi, A. B., Lozano, R., eds. World Health Report on Violence and Health. Geneva: World Health Organisation, 2002 http://www.who.int/violence_injury_prevention/violence/world_report/en/index.html Preventing Injuries and Violence: A Guide for Ministries of Health. Geneva: World Health Organisation, 2007 www.who.int/violence_injury_prevention/publications/injury_policy_planning/preven tion_moh/en/ WHO Global Consultation on Violence and Health. (1996) Violence: A Public Health Priority (WHO/EPA/SPI.POA.2). Geneva: World Health Organisation SOPH, UWC, Post Graduate Diploma in Public Health: Introducing Public Health: its Basis & Scope – Unit 2 160