IT ALL STARTS WITH AN EGG AND A SPERM:
advertisement

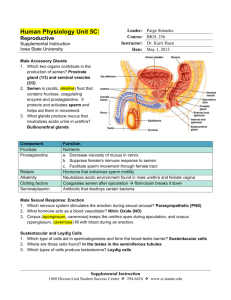
IT ALL STARTS WITH AN EGG AND A SPERM: NATURAL FERTILIZATION How does human fertilization occur? At first sight, a simple question – you’ve known the answer for years. Or you thought you did, because it’s not really as straightforward as that. A complicated biochemical and anatomical background underlies the process of merging a female egg and a male sperm to form what becomes a baby. An understanding of this background is especially vital for couples unable to conceive but who can be helped medically. THE FEMALE REPRODUCTIVE SYSTEM egg ovary fingerlike projections fallopian tube womb vagina 1 1| A woman’s reproductive organs. Frequently asked question Does ovarian stimulation affect the store of eggs resulting in early menopause? Find the answer on p. 80. THEORY A normal human female is born with about 300,000 to 400,000 eggs (also known as egg cells or ova) stored in two ovaries. She will produce no further eggs during her lifetime. On the contrary, a large number of these eggs die through a process of natural wastage, leaving about 100,000 to 200,000 by the time of puberty. The number remaining decreases over time until none are left, usually at the age of about fifty, which marks the onset of menopause. The ovaries normally release one ripe egg every four weeks during a woman’s fertile years. This is known as ovulation. Finger-like projections at the top of one fallopian tube catch the egg. The egg is ready for fertilization by a sperm (from the male) while it is inside the fallopian tube. Cilia (tiny hair-like projections) covering the inner wall of the fallopian tube gently waft the egg down to the uterus (or womb). Meanwhile, the lining of the uterus (the endometrium) has thickened in preparation for the arrival of an embryo. If the egg is not fertilized or the embryo fails to implant in the uterus, the mucous lining rapidly breaks up and is shed via the vagina. This process is known as menstruation (having a period). 13 THE MALE REPRODUCTIVE SYSTEM brains GnRH hypofyse FSH LH hypothalamus penis testosterone Testosterone testicle 2 bladder seminal vesicle vas deferens prostate gland urethra epididymis penis testicle 3 2| The hormonal ‘cycle’ of a man. 3| A man’s reproductive organs. THEORY 4| Testosterone Builder. Men who take testosterone in order to increase their muscle mass are giving an incorrect signal to their brain, i.e. that sufficient male hormone is present in the body. This leads to a halt in gonadotrophin production. But gonadotrophins are necessary for the production and maturation of sperm cells. Or how taking testosterone can lead to a significant reduction in sperm production and hence to infertility. 14 Sperm (spermatozoa or sperm cells) are produced in tiny tubes (tubules) inside the male’s testicles (testes). Sperm production begins in puberty and continues for the rest of a man’s life. Lesser known is the fact that sperm production and maturation is controlled by the same hormones that regulate women’s menstrual cycles: the gonadotrophins LH and FSH (see illustration 5 for the abbreviations). Together they stimulate the male reproductive organs (gonads) into the production and the ripening of sperm cells. Gonadotrophins are secreted by the hypofyse, a small gland in the brain which is controlled by the hypothalamus. The hypothalamus secretes at regular intervals a hormone called GnRH or Gonadotrophin Releasing Hormone, in a set rhythm dictating the release of FSH and LH. During the process of production and ripening of sperm the reproductive organs subsequently start to produce sex hormones. In the male, this is primarily testosterone. This is the hormone which turns a boy into a man. Production of this hormone begins at puberty, from which point on it controls the sexual function and libido of the man. Is is also responsible for the maturation of sperm cells. Production of testosterone peaks around the age of 30-35, then gradually begins to decline. In the male ‘cycle’, testosterone levels are 4 monitored in the brain. If sufficient levels are present, the secretion of GnRH slows down, resulting in a lower level of gonadotrophins produced. Similarly, if testosterone levels are low, e.g. because the testis are producing less, the brain gets the message that more FSH and LH are needed. In response the secretion of GnRH accelerates, causing more gonadotrophins to be released. The sperm cells’ itinerary As said before sperm cells are produced in tubules inside the testicles. The production itself is a complicated process of cell division and cell differentiation which takes about three months in total. But of course the process occurs in thousands of tubules and at different stages constantly, so that there is always a supply of mature sperm available. After its production in the testicle, the sperm travels to the epididymis, which consists of one long, tightly coiled tube. The sperm remains here for about a week, during which it continues to mature and become more motile. The epididymis also serves as a reservoir. During an orgasm, sperm cells are expelled from the epididymis and set out on their journey to the outside world via the vas deferens. On their way out they are mixed with a nutrient-rich plasma from the prostate and seminal vesicles. They are then ejaculated trough the urethra in the penis. A normally fertile man will ejaculate between 1.5 and 4 ml of semen containing some 20 to 200 million sperm per ml. See the World Health Organisation (WHO) overview for other standards which ‘normal’ sperm must meet. Semen reaching the vagina undergoes a drastic transformation within less than half an hour, changing from thick and sticky to thin and fluid. Large numbers of sperm simply flow out of the vagina, while most of the rest cannot get past the mucous around the cervix (neck of the womb). A few hundred sperm at most – motile and well-formed sperm – succeed in entering the uterus and climbing to reach one of the fallopian tubes. If a ripe egg is waiting there, there is a chance it will be fertilized – in principle by a single sperm. Normal sperm according to WHO-norms Semen volume 2,0 ml or more pH 7,2 – 7,8 Sperm concentration 20 million/ml or more total count 40 million or more progressive motility (fast or slow forward movement) > 50% or fast progressive motility > 25% normal formation > 30% vitality > 50% live white blood cells < 1 million/ml brain GnRH pituitary gland FSH LH THE MENSTRUAL CYCLE ovary A normal menstrual cycle lasts four weeks, although this time may vary greatly from one woman to another and one cycle to another. A menstrual cycle begins with the ripening of an egg and ends in a period (menstruation) or pregnancy. oestrogen From day one to ovulation (follicular phase) mucos lining progesterone womb 5 GnRH (Gonadotrophins Releasing Hormone): encourages the menstrual cycle. FSH (Follicle Stimulating Hormone): develops the follicles in the ovaries. LH (Luteinising Hormone): encourages ovulation. hCG (Humane Chorion Gonadotrophin) or pregnancy hormone: supports the further development of the embryo into a baby. 5| Hormones involved in the menstrual cycle and/or the IVF-treatment. THEORY The menstrual cycle is triggered by a low level of oestrogens (female hormones) in the blood. This causes the hypothalamus, a neural control centre at the base of the brain, to secrete GnRH (see illustration 5). GnRH stimulates the pituitary gland, the master endocrine gland located below the hypothalamus, to produce follicle stimulating hormone (FSH) and luteinising hormone (LH). These two hormones directly stimulate the woman’s reproductive organs (gonads) and are therefore called gonadotrophins. GnRH causes them to be ‘released’: hence the name Gonadotrophins Releasing Hormone. FSH stimulates the development of several ovarian follicles, small sacs in the ovaries filled with liquid and each containing an egg. Oestrogens secreted by these follicles cause the endometrium to thicken in preparation for the possible implantation of an embryo. Oestrogen secretion by the follicles causes oestrogen levels to rise, hypothalamus 15 sending a message to the brain to slow down the release of GnRH. As a result FSH production is reduced too, which stops further follicle development and causes all but one to die. Nevertheless there is always one dominant follicle that survives by adapting to the low FSH levels, and this follicle alone continues to grow. Under the influence of FSH and LH the egg in the dominant follicle ripens. When oestrogen levels are sufficiently high an LH surge occurs (a sudden increase in the amount of LH released), causing final maturation of the egg. The egg is now mature and ovulation can take place. There are approximately 12 to 40 hours between the LH surge and ovulation. The LH surge occurs around day 12 of a 28-day cycle, with ovulation occuring at around day 14. MENSTRUAL CYCLE Maturation of the egg within the follicle Ovulation LH surge Luteinising hormone Progesterone FSH Oestrogens MEN STRUAL C YCLE Endometrium Days 4 8 12 16 Ovulation 20 24 DAY 28 6 1 14 28 fallopian tube FOLLICU L AR PHASE Maturation of the egg in the follicle LUTEAL PHA S E Possible fertilization followed by possible implantation OVU L ATION follicle egg PR EG NANT OR M E N STRUATION 7 From ovulation to day 28 (luteal phase) After ovulation, the ripe egg travels through the fallopian tube to the womb. The remaining empty follicle in the ovary turns into a yellow glandular mass of tissue (corpus luteum). This does not only secrete oestrogens (as the follicle did) but also progesterone. Together these hormones stimulate the endometrium to thicken as well as suppressing the production of FSH and LH by the pituitary gland. ovulation Pregnancy yellow mass of tissue 8 6| Hormonal changes during the menstrual cycle. 7| Graphice representation of the menstrual cycle. In practice, ovulation is not that easy to predict. THEORY 8| From follicle to yellow mass of tissue. 16 An egg may be fertilized up to about one day after ovulation. A sperm retains its ability to fertilize an egg up to around two days after ejaculation. Thus, a woman has three days of effective fertility per cycle. Fertilization takes place when the spermatozoa, having reached the distal portion of one tube, succesfully penetrates into the egg, this creating an embryo. The fresh embryo is then undergoing successive divisions and is transported during a six day period towards the uterine cavity. By then it has become a blastocyst (multi-cellular germinal vesicle). It implants in the uterine mucosa and starts to secrete hCG. This hormone can be identified in female blood (or urine), which makes diagnosis of pregnancy possible. During the first trimester hCG acts on the corpus luteum, which then continues to produce oestrogens and progresterone. During early pregnancy (first trimester) this hormonal cooperation sustains embryo development. This function is subsequently taken over by the placenta, an organ which sees to the nutritive exchanges between mother and foetus. By that time, the evolution of the pregnancy has become autonomous. Menstruation If pregnancy does not occur, the corpus luteum will begin to break down about ten days after ovulation. This causes the oestrogen and progesterone levels to fall sharply, leading to the shedding of the endometrium at around day 28 of the menstrual cycle. The woman then menstruates, and the secretion of GnRH by the hypothalamus and of FSH and LH by the pituitary gland begins all over again. The first day of menstruation is also the first day of the new menstrual cycle. This is why the timing of the IVF treatment is always counted from of the first day of (red) bleeding (= day 1). THEORY 17 GIVING NATURE A HELPING HAND: IN VITRO FERTILIZATION If pregnancy through the usual method is not possible for you, artificial insemination (see further, p. 53) or in vitro fertilization (IVF) may be the solution. REDUCED FERTILITY weg van de zaadcellen 9 10 9| The itinerary of the sperm cells through the male … THEORY 10| … and thereafter through the female genital organs. 18 Our knowledge of the human reproductive system and the hormones which control it, teach us also what can go wrong: • defective hormone production in the brain; • defective hormone production in the reproductive organs; • insufficient production of sperm cells; • poor quality of sperm; • problems related to the ripening process of egg cells; • insufficient supply absence of eggs, poor quality of eggs; • obstructions in the path of the sperm within the male reproductive system; • patency of the fallopian tubes; • incorrect timing or location of the unity between sperm and egg; • implantation problems of the embryo. We distinguish different causes of infertility: • gynaecological causes: i.e. the woman’s fallopian tubes are blocked or her uterus has certain malformations; • hormonal indications: i.e. ovulation does not occur or is disturbed; • andrological indications: the man doesn’t produce (enough) healthy sperm cells; and • immunological indications: man or woman produce spermneutralising antibodies Furthermore certain couples still aren’t expecting a child after having regular sexual intercourse without any form of birth control for a year or two, with the doctors failing to identify any discernable cause. These cases are called idiopathic or unexplained infertility. 12 11 THE TREATMENT IN A NUTSHELL An IVF treatment is designed to help couples who suffer from one or more of the aforementioned fertility problems. The natural menstrual cycle will then be temporarily replaced by a medically induced cycle. Treatment begins with hormonal stimulation of the woman’s ovaries. The aim is to produce several eggs in the course of one menstrual cycle. The ripe eggs are harvested (egg pick-up) from the ovaries just before ovulation, using a very fine hollow needle. They are then mixed in the laboratory with selected sperm provided by the man. This may even be one single sperm cell, which is injected directly in the egg. In this case we talk about ICSI. If all goes well, some of the eggs will be fertilized and begin to develop into embryos. One or two embryos are then transferred to the woman’s uterus (embryo transfer), where we hope one will implant itself and grow into a healthy baby. In the past, two or three embryos used to be transferred, to increase the chances of a successful implantation. However, the chances of a multiple pregnancy (twins, triplets) are also increased. Improved medical techniques often allow the transfer of only one embryo nowadays, thus eliminating the chances of a multiple pregnancy, and at the same time reducing the general health risks for woman and child. Any remaining good quality embryos are frozen and stored for later use if the first attempt does not result in pregnancy or if the woman wishes to have more children later. This avoids unnecessary further stimulation of the ovaries and subsequent procedures. Chances of a successful transfer are proportional to the number of thawed embryos because they don’t all survive the thawing process. Even if they are all of a good quality, the survival rate is fifty percent on average. So it is perfectly possible that a couple has embryos from a previous treatment, but still has to repeat the entire IVF treatment for another attempt or for a second child. 13 14 11| Egg cumulus: the egg is in the top right-hand corner surrounded by feeding cells. 12| Sperm under a microscope. 13| Eggs and semen are mixed in a glass dish (classic IVF). 14| Insemination via ICSI: the sperm is sucked into a needle and injected into the egg. THEORY 19 Not easy but not painful either In vitro fertilization is both a minor and a major treatment. Physically, the demands are relatively small in that IVF involves a series of minor, low-risk procedures, usually with little or no pain. The drugs used may cause some short-term discomfort, but these side-effects are not serious or lasting. Moreover IVF treatment is an out-patient procedure and does not require you to stay overnight in UZ Brussel. However, IVF does make great mental demands on a couple. The treatment involves many procedures and special routines and will require a few (temporary) changes to your normal lifestyle. Of course, you are certain to feel some stress, uncertainty and worry; this is all quite natural and is focused on one crucial question: will the treatment be successful? The effects of this will place a heavy psychological burden on you, and you may find it extremely wearing. The CRG at UZ Brussel tries to give each couple every help and guidance they may need. Helping you to satisfy your natural desire for a child and ensuring your comfort during the treatment are both very high on our list of priorities. PREGNANCY IS NEVER A CERTAINTY 15 16 15| Fertilized egg, the day after IVF, still surrounded by sperm. THEORY 16| If everything goes well, the end result is pregnancy. 20 The most important conclusion from practical experience is that your individual chances of success are very difficult to predict beforehand. Apart from the age of the woman the type of treatment, the cause of the fertility problem, and chance play a role. Sometimes the exact same treatment will produce results after the second or third attempt. Why not the first time is not always determinable. That is why counsellors nor doctors will respond to questions about the chances of success of an individual treatment. The risk to create unrealistic expectations – or on the contrary erroneously stifle justified hope – is too great. Based on our extensive experience for many years standing and after examination of both partners we can of course give you a general idea as to what the odds are. We’ll always try to assess your medical chances as accurately as possible. On the whole we can affirm that IVF/ICSI certainly is worth a try for many couples, but that it doesn’t necessarily always results in the birth of a child. Statistic chance of delivery 100 1 2 3 4 5 6 7 8 90 The average chance of success of an IVF treatment is closely related to the woman’s age, as can clearly be seen in this graph. 80 70 Number of expected deliveries (out of 100 women) 60 50 20–29 age 40 30–34 age 35–37 age 30 average > 20–37 age 38–39 age 20 40–43 age 10 > 43 age 0 Number of fertilization cycles (IVF or ICSI) This graph shows the relation between the expected percentage of deliveries (not pregancies!), the woman’s age and the number of IVF or ICSI attempts. The vertical axis shows how many women (out of a hundred) of what age may give birth to a baby after an IVF or ICSI treatment; the horizontal axis shows after how many attempts. Example: of the 100 women in the 20 to 29 age group who started with IVF – ICSI, 37 may be expected to have given birth to a baby after the first attempt, 60 after the second attempt and 73 after the third attempt. In terms of ‘average’ success – i.e. all ages and irrespective of the number of attempts – the following figures are available. Of 3,600 pick-ups performed in the course of one year by the CRG at UZ Brussel, nearly 90% produce eggs which are fertilized to become viable embryos ready for transfer to the uterus. These embryo transfers produce a pregnancy in 30 percent of cases on average. So almost 25% of the original pick-ups result in the live birth of a baby. THEORY 21