Demand Exceeds Capacity
advertisement
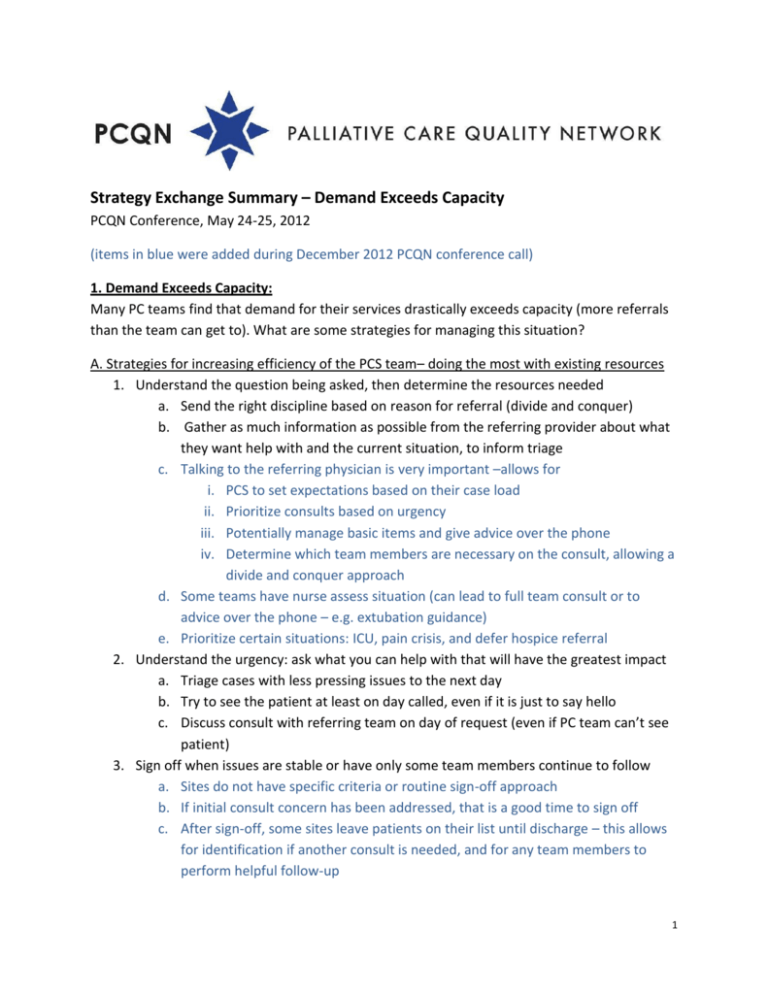
Strategy Exchange Summary – Demand Exceeds Capacity PCQN Conference, May 24-25, 2012 (items in blue were added during December 2012 PCQN conference call) 1. Demand Exceeds Capacity: Many PC teams find that demand for their services drastically exceeds capacity (more referrals than the team can get to). What are some strategies for managing this situation? A. Strategies for increasing efficiency of the PCS team– doing the most with existing resources 1. Understand the question being asked, then determine the resources needed a. Send the right discipline based on reason for referral (divide and conquer) b. Gather as much information as possible from the referring provider about what they want help with and the current situation, to inform triage c. Talking to the referring physician is very important –allows for i. PCS to set expectations based on their case load ii. Prioritize consults based on urgency iii. Potentially manage basic items and give advice over the phone iv. Determine which team members are necessary on the consult, allowing a divide and conquer approach d. Some teams have nurse assess situation (can lead to full team consult or to advice over the phone – e.g. extubation guidance) e. Prioritize certain situations: ICU, pain crisis, and defer hospice referral 2. Understand the urgency: ask what you can help with that will have the greatest impact a. Triage cases with less pressing issues to the next day b. Try to see the patient at least on day called, even if it is just to say hello c. Discuss consult with referring team on day of request (even if PC team can’t see patient) 3. Sign off when issues are stable or have only some team members continue to follow a. Sites do not have specific criteria or routine sign-off approach b. If initial consult concern has been addressed, that is a good time to sign off c. After sign-off, some sites leave patients on their list until discharge – this allows for identification if another consult is needed, and for any team members to perform helpful follow-up 1 4. If referrals relate to symptom management but no MD/NP on service (that day) identify and utilize non-PC MDs who can provide backup 5. Rather than one-size fits all standard intervention/process, consider patient needs identified through standardized intake/evaluation and adjust intervention accordingly– does the patient need to be seen today? Daily? By which members of the team? 6. Consider changing staffing to match periods of highest demand, for example, from 1.0 FTE 24/7 to 2.0 FTE 5d/week B. Strategies for reducing demand/empowering other providers 1. Be specific about the scope of care for your service and which patients should be referred for which reasons 2. Triage to outpatient setting a. Refer to outpatient clinic for follow-up instead of inpatient consult b. Ensure good follow-up post discharge to avoid readmissions c. Integrate PC into other programs (eg, Onc clinics, geriatric practices, etc) d. Triaging to a clinic doesn’t work well if the inpatient team hasn’t connected with the patient (One site has experience with this) – the patients don’t fully understand PC and tend to not show up at outpatient appointments – performing a ‘meet and greet’ seems to alleviate this challenge e. Referrals come in almost at the point of discharge and the social worker follows up via phone with the family after discharge in the outpatient setting f. Tie inpatient and outpatient services very closely – begin building the outpatient relationship/services before discharge for continuity of care 3. Use hospital staff not on PC team if they can meet that patient’s need (eg, SW consult vs PC team consult) 4. Provide sufficient education to obviate consultation a. Teach the skill/solution to other staff: MD, RN, SW, chaplain C. Strategies for increasing resources 1. Make the case for how the PCS lowers costs and promotes efficient resource utilization 2. Prove the need – track PC team hours and activities for 1-2 weeks to show how much effort is required to manage current case load and that there is no additional capacity to accommodate more consult requests a. Positive perception was very helpful – showing high physician satisfaction, high patient satisfaction, high consult numbers 2 b. Analysis that demonstrated cost savings with palliative care consultation for ICU patients allowed for support for a new ICU-based PC team at one site (improving ICU utilization was goal for this hospital) 3. Consider capping service. Establish a maximum number of new consults per day or week and send administration a weekly email regarding the excess demand, number of patients the team was not able to see, and collect data on patients not seen a. One site capped by week – this posed challenges with rush of consultation requests at the beginning of the week when cap hadn’t been reached yet and sometimes patients were seen that would have been lower priority simply because they were earlier in the week. Capping was eliminated when more staff was added b. Challenge with capping was that saying ‘no’ was very challenging – this isn’t the way to build a service c. PCS Patients/FTE (see below and in reference*) Total FTE RN/NP, MD FTE RN/NP, MD, SW, Chaplain Average Annual Census 188 258 “Able to Cope” 133 190 “Struggling to Cope” 220 297 *Pantilat SZ, Kerr KM, Billings JA, Bruno KA, O'Riordan DL. Characteristics of Palliative Care Consultation Services in California Hospitals. J Palliat Med. Mar 6 2012;15(5):555-560. d. Some sites implement a daily service cap based on numbers and complexity and roll over consultation requests over to the next day e. Catch 22 – desire to see as many patients as possible and all requests received, but if the service is too busy, quality suffers D. General observations about environment/challenges 1. Spend time, do the work, work hard, stay late occasionally if needed, but also keep boundaries a. Do not let people burn-out – time management, self-care, and limits are important 2. Try to be helpful to every person who consults the PCS tam in order to preserve referral base, but don’t sacrifice the team 3