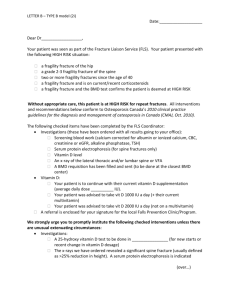
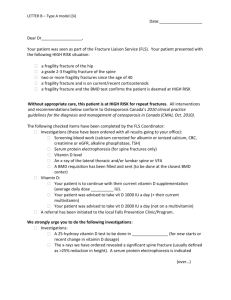
Case study of a patient with osteoporosis
advertisement
How to use Clinical Evidence to inform clinical decision making A case study using the CE review on fracture prevention in postmenopausal women Osteoporosis Case study constructed for purpose of Clinical Evidence demonstration. Not based on a patient seen by the author, or on any particular individual • Case history: 68-year-old white woman • Presents to accident and emergency department with right wrist pain, swelling, and displacement following a fall onto outstretched hand on the stairs at home History • Past medical history – asthma since childhood (treated with corticosteroids aged 50–55), gastric ulcer aged 45, menopause age 59, left wrist fracture aged 67 • Family history – stroke in sister aged 65, hip fracture in mother aged 78. Mother diagnosed with osteoporosis • Social history – lives alone, 2 children, retired, smokes 5 cigarettes per day, occasional alcohol, takes no exercise, fully mobile and able to complete all ADLs (activities of daily living) Examination • On examination – wrist displaced, swollen, no open wound • No loss of sensation or vascular compromise • X-ray – Colles’ fracture of distal radius present N.B. The most common osteoporotic fractures are vertebrae, wrists, and hips. Lifetime risk of fracture in white women is 20% for spine, 15% for wrist, and 18% for hip. There is an exponential increase in fracture over 50 years Investigations and treatment for presenting problem • Colles’ fracture treated conservatively with cast and analgesia • DEXA scan arranged as postmenopausal woman with history of previous fracture, corticosteroid use, and family history of osteoporosis – osteoporosis diagnosed in this patient Further issues for you to consider... • How can further fractures be prevented? • Bisphosphonates are the most commonly used treatment, but how useful are they? • Are there any non-pharmacological treatments that would help? • Which of these options are most appropriate for this particular person? • How strong is the evidence for these options? Bisphosphonates Clinical question Categorisation of effectiveness for each bisphosphonate we cover Different bisphosphonates for which we have searched for systematic review or randomised control trial evidence Click on the drug of interest to see the evidence base for the benefits and harms… … for example, alendronate Here there is a summary of alendronate compared with placebo, and with other antiresorptive drugs Scrolling down further shows the evidence base behind these statements Here we can see the quality of the evidence we have available to make decisions on. Clicking on the GRADE table shows how these quality assessments were decided on … GRADE table This column shows the number of studies and participants that the GRADE statement is based on Here, the evidence was RCTs or SRs, gaining a maximum of 4 points. The GRADE depends on the final score once the numbers in the table row are added together. A score of 4 means high-quality evidence; 3 is moderate-quality, 2 is low-quality, etc These 3 table rows focus on alendronate In the ‘comments’ column we explain what we deducted or added points for Other pharmacological treatments Just as with bisphosphonates, click on the question about other pharmacological treatments to see this summary table, and then click on individual drugs to see how they compare with placebo and each other in terms of benefits and harms Non-pharmacological treatments … and the same for nonpharmacological treatments! Click on these icons to read about our categorisation of interventions: they are based on a system derived by the Cochrane Collaboration Pregnancy and Childbirth group Individual medicine • Thinking about this person: • Past medical history – previous fracture, postmenopausal, corticosteroid use, gastric ulcer • We can see from the review that alendronate, (and other bisphosphonates) are associated with gastric ulcers and erosions • Therefore, we should consider other options, but remember as well that this is not a contraindication, but a caution about their use Family history – stroke (raloxifene may increase stroke risk) What would be better? Using Clinical Evidence to help answer the patient’s questions… • Questions your patient has… • Several friends take HRT and have recommended this – should she do the same? • At present, she does not take any regular exercise, but wonders whether this is important. She has heard that exercise ‘strengthens the bones’, but is worried about having a fall and getting another fracture • Since the diagnosis she has been taking calcium and vitamin D supplements as she hoped these would reduce her fracture risk – are these a good use of money and are they harmful in any way? HRT This may help answer the patient’s questions about exercise. Although exercise has other beneficial effects, the evidence here shows that, contrary to media reports, there is not enough high-quality evidence to know whether or not this is the case From the ‘Key Points’ section, we see that although HRT may reduce fractures, the risks of adverse effects are thought to outweigh the benefits. From this, you can advise the patient of this, and suggest that there are other options that are as effective but safer Calcium and vitamin D are covered in the Key Points, but the patient would like further information… The patient was keen to find out more about calcium versus vitamin D. She also wanted to know whether there was any harm in continuing to take calcium supplements in the absence of good evidence for their use Remember that you can also find patient information leaflets on the Clinical Evidence website Conclusions • Risks of HRT outweigh the benefits • We don’t know if exercise is beneficial • Monotherapy with calcium or vitamin D has not been shown to reduce fractures • Bisphosphonates are effective but are associated with gastric ulcers • Raloxifene increases stroke risk