cauti 101 - K
advertisement
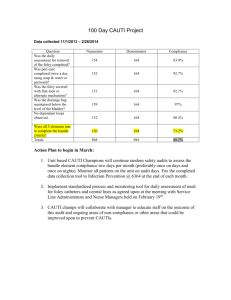
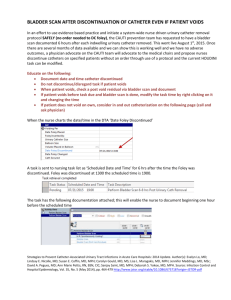
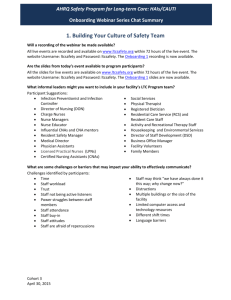
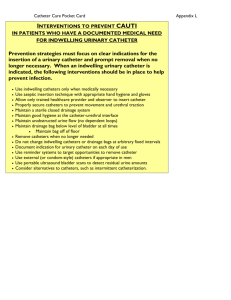
Deborah R. Campbell, RN-BC, CCRN, MSN Pediatric Cardiovascular CNS Kentucky Hospital Association Children’s Hospital Association QTN faculty Clinical Consultant for Carefusion ◦ Work to be presented was completed without commercial support Review evidence based interventions to prevent CAUTI Discuss bundle concept as relates to CAUTI prevention Discuss CAUTI prevention as a team sport Discuss ‘safety culture’ aspects of CAUTI prevention Sterile insertion technique (Consider a kit) ◦ Smallest, softest catheter that will do the job Ensure adequate hydration Hand hygiene Perineal care ◦ BID with soap and water, PRN BM (Products) Keep bag below the level of bladder Prevent bag, tubing from touching floor Avoid dependent loops, kinks No disruption of closed system Obtain specimens using aseptic technique ◦ Only if absolutely necessary ◦ Remove and replace for C&S Empty the bag when1/2-2/3 full (Q4hrs?) Each patient should have own graduated cylinder Daily observation for signs, sx of UTI Isolation of diagnosed CAUTI pt from anyone with a catheter Utilize a securement device Bladder scanning- non-invasive, easy, quick Intermittent catheterization v. in-dwelling caths- better for patient, more work for staff Ditch the bath basins CHG baths- microbe burden Appropriate nurse staffing Antibiotic or silver-coated catheters Hydrogel catheters- discourage biofilm adherence Catheter valves- store urine in bladder v. bag ◦ More physiologic as well, decreases need to re-train Is there a “magic bullet? Are there certain, specific items 1+1=3 Synergy? Pathogen dose v. immune response Bundles act as checklists Bundles act as curriculum Recipe v. culture Policy change is not = to practice change QI 101- Educate, Implement, Audit, Improve, SUSTAIN All at once or step-wise? How do I choose from the menu? ◦ ◦ ◦ ◦ Problems known to exist at your place Acceptable to your front line staff Ways to measure already in place (LAST) RCAs on CAUTIs that occur Is there a best way? ◦ Direct Observation Peers Supervisors, educators, CNSs ◦ Self-audits ◦ Secret Shoppers Sampling ◦ Include weekends, nights ◦ Attempt randomness by setting specific days, times Met your goals consistently, decrease frequency-BUT never less than quarterly. Make the right action the default ◦ ◦ ◦ ◦ ◦ Opt-outs v. necessity to overtly choose Nurse driven protocols Standardization Redundant processes From the IHI- Everyone chooses (or is assigned) a focus area for which they provide input 5 audits per day per person (on HAPU, CLABSI, CAUTI, SSI or VAP) Care team members other than primary RN ◦ ◦ ◦ ◦ ◦ ◦ ◦ Nurses helping out (regular, floated, agency) PCAs X-ray technicians Respiratory therapists Transporters Family members Patients themselves Decrease the number of insertions/transfers with catheters ◦ ED ◦ OR Success is possible! ◦ Emergency room staff education and use of a urinary catheter indication sheet improves appropriate use of foley catheters. Presented by RM Gokula, MD, MA Smith, MD, and J Hickner, MD, Lansing, Michigan Can’t define it, but we know it when we see it ◦ Non-heirarchical ◦ Healthy team dynamics First names Safe to question, interrupt (Scripting!) ◦ Patient-Centered ◦ No blame-it’s all about the process ◦ Personal accountability (1 patient, 1 action at a time) Link participation to annual evaluations Build concept that patient well-being is everyone’s responsibility ◦ Individual ◦ Team ◦ No carve-outs Rules apply to everyone, regardless of discipline Think pro-actively- “what could harm this patient today?” Effective for more than one outcome ◦ Infections ◦ Unplanned device removals ◦ Med Errors Videos, e.g. Josie King Think of patient in front of you being your mother, grandfather, child VA campaign ◦ “Have you ever killed someone with your bare hands?”