External defibrillation
advertisement
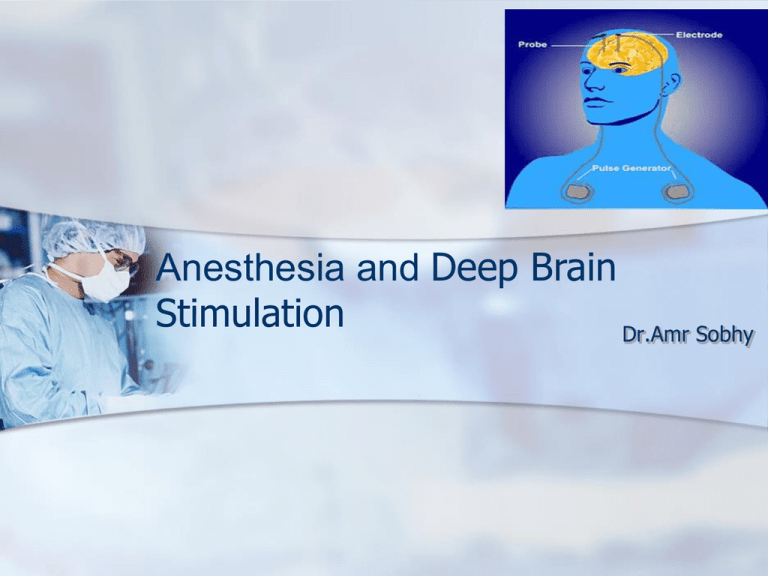
Anesthesia and Deep Brain Stimulation Dr.Amr Sobhy Objectives Brief History Indications and contra-indications The DBS surgical procedure Anesthetic consideration Anesthetic technique Safety issues Brief History Basal ganglia have been targeted for neuromodulator surgery since the 1930s. 1950s: Pallidotomy was the accepted procedure for the treatment of Parkinsonism Disease (PD). procedures were irreversible and were associated with several permanent side effects. With the advent of L-dopa (1968),this surgery largely stopped. Limitations of dopaminergic therapy led to a resurgence of new surgical techniques directed at basal ganglia targets in early 1990s. Brief History 1993: Bilateral high-frequency stimulation of subthalamic nucleus (STN) introduced in treatment of advanced PD Pioneering studies & empirical observations during surgery showed that DBS improved PD patient’s motor function and quality of life. Today, DBS has become a non-lesioning alternative to pallidotomy. What is DBS? A surgically implanted medical device called a brain pacemaker. Sends electrical impulses to the brain. Traditionally used to treat movement disorders such chronic pain, Parkinson’s disease, tremor, and dystonia. as Mechanism The exact mechanism is incompletely understood . may differ depending on the site of stimulation, The primary target sites : 1. 2. 3. Vim = ventralis intermedius nucleus of the thalamus GPi = posteroventral portion of the internal segment of the globus pallidus STN = subthalamic nucleus Mechanism stimulation of the STN causes hyperpolarization or “neuronal jamming,” and this consequentially results in the inhibition of its activity. Stimulation of the GPi nuclei may result in activation (GABA)ergic axons, which in turn inhibits GPi neurons. In contrast, stimulation of the Vim nucleus of the thalamus activates output to the neurons in the reticular nucleus, which then sends inhibitory efferent back to the thalamic nuclei. Contra-indications patients clearly have to be fit enough to undergo the surgery and well enough to benefit from it. The major concern is of coagulopathies, as this would increase the risk of hemorrhage with the electrode insertion Components Three Major Components Implanted pulse generator (IPG) Lead battery-powered neurostimulator encased in a titanium housing, which sends electrical pulses to the brain to interfere with neural activity at the target site coiled wire insulated in polyurethane with four platinum iridium electrodes and is placed in one of three areas of the brain Extension insulated wire that runs from the head, down the side of the neck, behind the ear to the IPG, which is placed subcutaneously below the clavicle or in some cases, the abdomen The DBS surgical procedure The DBS surgical procedure Precise implantation of stimulation electrode in targeted brain area. Connecting electrode to programmable pulse generator internal The DBS surgical procedure Pre-Operative Stage: Stereotactic Surgery - Locate targeted brain areas Stereotactic frame MRI, CT, or ventriculography Stereotactic atlas The DBS surgical procedure Pre-Operative Stage: Functional Stereotactic Surgery - Electrophysiological exploration of targeted regions via test electrodes - Involves: 1. Microrecording 2. Test-stimulation The DBS surgical procedure Electrode-Stimulator Connection: Electrode Extension (passed under skin to chest) Chest: Battery-operated stimulator Patient turns stimulator “on” and “off” by passing magnet over the skin overlying stimulator Typical stimulator settings: - Voltage amplitude: 2-3 V - Pulse width: 90 μs - Stimulation frequency: 130-185 Hz Anesthetic consideration 1- Patient-related considerations Primary disease (Parkinson disease, dystonia, essential tremors, chronic pain, and epilepsy) Comorbid medical conditions of patient and of disease Age (children and elderly) Appropriate patient selection and preparation Polypharmacy and altered pharmacokinetics and dynamics Potential drug interactions Medication “off state”— worsening of symptoms Anesthetic consideration 2- Procedure-related considerations Different locations of patient care (magnetic resonance imaging and operating room) Use of a stereotactic frame: potential for difficult airway Positioning of patient on the operating room table: difficult with movement disorders Semisitting position: risk of venous air embolism and hypovolemia Blood pressure control: prevention of hemorrhage from hypertension during electrode insertion Anesthetic consideration Microelectrode recordings: anesthetic effects may impair Macro stimulation testing: need for an awake and cooperative patient Long duration of procedure: patient fatigue Complications: airway obstruction, seizures, neurologic deterioration, and hypertension Anesthetic technique Anesthetic management Stage of Framing Overall, the majority of patients tolerate the insertion of DBS using a combination of local anesthesia and sedation/analgesia infusion of dilute Remifentanil usually 0.02–0.05 mg/ kg/ min OR Dexametamedonie usually 0.40.7µg/ kg/ h Oxygen is provided by a microphone supply attached to the underside of the frame, and music of the patient’s choice played to aid relaxation. Anesthetic management Stage of Imaging the anesthetist is equipped with the tool to remove the fixing screws, in case the frame needs to be removed for access to the airway Anesthetic management Stage of implantation Awake: an infusion of remifentanil as above, while full monitoring and supplemental oxygen is provided. Benzodiazepines are avoided G.A: typically a target-controlled infusion of propofol and remifentanil and a non-depolarizing neuromuscular block technique is used. If the patient has Parkinson’s disease, then it is prudent to insert a nasogastric tube Safety Issues G.A & R.A avoiding drugs with extra-pyramidal side-effects in this group of patients. . Peripheral nerve stimulators can still be used MRI scanning Heating, Magnetic field interactions and DBS function This can produce Unintended stimulation thermal lesions possibly resulting in coma, paralysis, or death. contraindicated Safety Issues Diathermy Can damage the DBS leads and can also cause temporary suppression of the neurostimulator. use bipolar diathermy. if unipolar diathermy is necessary: (a) use only a low-voltage mode. (b) use the lowest possible power setting. (c) keep the current path (ground plate) as far from the neurostimulator (d)After using diathermy, confirm that the neurostimulator is functioning as intended Safety Issues External defibrillation position defibrillation paddles as far from the neurostimulator as possible. position defibrillation paddles perpendicular to the implanted neurostimulator-lead system. use the lowest clinically appropriate energy output. Confirm that the DBS is functioning correctly after any external defibrillation. Safety Issues Electroconvulsive therapy ECT may be a safe and effective option. Care in placing the ECT electrodes. Switching the DBS off before ECT. Limiting the number of ECT sessions should be considered. Any Questions? summary DBS is the pace maker of the brain. Anesthetic consideration of PD during insertion should be consider especially withholding of the drugs and early resume postoperatively. Dealing with patient have DBS devise need especial care as regard electromagnetic interference (MRIDiathermy-External defibrillation). Thank you