Uploaded by
KRIZZEA ANNE TUPPAL
Exploratory Laparotomy Case Analysis: Gastric Ulcer Disease

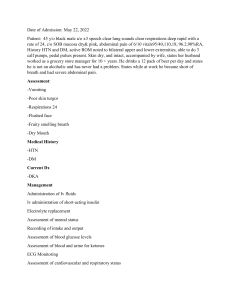
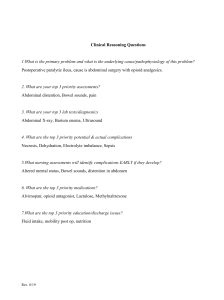
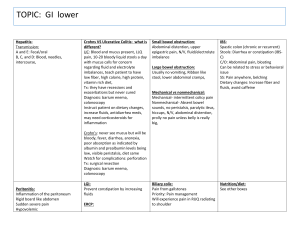
Case Analysis of Exploratory Laparotomy (Ex-Lap) Submitted by: Tuppal, Krizzea Anne A. BSN4-NDC5 Submitted to: Mrs. Chariz Hazel Anne, RN TABLE OF CONTENTS Chapter I: Introduction………………………………………………………………………4 Chapter II: Patient’s History and Background……………………………………………. .10 Chapter III: Presenting Signs and Symptoms………………………………..…………… .12 Chapter IV: Initial Assessment and Diagnostic Tests………………………………………17 Chapter V: Pathophysiology of the Disease……………………………………………….22 Chapter VI: Laboratory Results……………………………………………………………25 Chapter VII: Nursing and Medical Management…………………………………………26 a. List of Identified Problems b. Prioritization c. Nursing Care Plan d. Drug Study Chapter VIII: Summary and Conclusion……………………………………………………39 INTRODUCTION This case study focuses on Patient X, a 55 year-old male diagnosed with Gastric Ulcer Disease with Peritoneal Contamination. Patient X was admitted to the hospital on March 31, 2025 and received care from student nurses and the medical team. Prior to admission, Patient X experienced sudden severe abdominal pain and showed signs of peritonitis to which the patient had undergone an exploratory laparotomy where they found a perforated ulcer with peritoneal contamination. The patient received palliative care management within the shift and his stay in the facility. Exploratory Laparotomy is a medical procedure performed with the objective of obtaining information that is not available via clinical diagnostic methods. It is usually performed in patients with acute or unexplained abdominal pain, in patients who have sustained abdominal trauma, and occasionally for staging in patients with a malignancy. Common indications for performing an exploratory laparotomy include Acute and Chronic Abdominal Pain, Abdominal Trauma, Obscure Gastrointestinal Bleeding, Staging of Ovarian Malignancy and Hodgkin Disease, Peritonitis, Ectopic Pregnancy, Post Operative Complications and Infections. The management of a perforated viscus begins with rapid assessment and stabilization. Patients often present with signs of shock, such as hypotension and tachycardia, due to fluid loss or septic shock. Initial treatment includes fluid resuscitation with IV fluids to restore volume and maintain blood pressure, along with pain management using analgesics and oxygen therapy to ensure adequate oxygenation. Vital signs are closely monitored, and imaging studies help confirm the diagnosis. Laboratory tests assess infection severity and organ function. Broad-spectrum antibiotics are administered immediately to cover both aerobic and anaerobic organisms, and treatment is adjusted based on culture results. Surgical intervention is essential, with laparotomy being the typical approach for urgent cases. If the perforation is small and localized, laparoscopy may be used. The surgeon repairs the perforation, often with primary closure or an omentum patch in cases like gastric perforation. For extensive damage, bowel resection or diversion may be required. Peritoneal lavage is performed to irrigate the abdomen, and drains may be placed to prevent fluid accumulation and infection. After surgery for a perforated viscus, the patient requires close monitoring for complications such as infection, abscess formation, or sepsis. Critical patients may be transferred to the ICU for intensive surveillance, especially if they need mechanical ventilation or vasopressor support. Postoperative antibiotic therapy continues for several days or weeks, tailored to the patient's condition and culture results. Nutritional support is essential, with early enteral feeding encouraged if possible, or parenteral nutrition if bowel function is delayed. Continuous monitoring of fluid and electrolyte balance is crucial, as imbalances are common in the recovery period, particularly after bowel resections or in septic patients. Patient Information: Name: Patient X Age: 55 years old Sex: Male Medical History: A history of Peptic Ulcer Disease Chief Complaint: Sudden severe abdominal pain and signs of peritonitis PATIENT’S HISTORY & BACKGROUND Patient X has a history of Peptic Ulcer Disease to which he has not properly managed by not modifying his lifestyle. Patient’s previous medications are Proton Pump Inhibotors, H2 Blockers, Antacids which he uses to reduce his gastric acid production. Antibiotic Therapy for H. pylori eradication and discontinuation of NSAIDs or other medications that may exacerbate ulcers. PRESENTING SIGNS AND SYMPTOMS Patient X’s vital gigns are as follows which his is BP= 90/50 PR= 128 bpm RR= 28 bpm and SPO2= 95%. The patient experienced sudden onset of severe and sharp abdominal pain and showed signs of peritonitis. Patient X described pain as stabbing or burning and the worst pain he has ever experienced. Pain radiates to the back, right shoulder, and chest. Pain also increases with movement, coughing, and deep breathing. Upon assessment, Patient’s abdominal muscles is tense and rigid which is commonly known as "board-like" abdomen. Tenderness increases when the abdomen is pressed and released. Patient also experienced nausea and vomiting. INITIAL ASSESSMENT & DIAGNOSTIC TESTS Diagnostic/Laboratory Findings: a. Contrast-Enhanced CT Scan revealed a gas within the abdominal wall. There is also a presence of abscess in the peritoneal cavity. b. Complete Blood Count revealed elavated WBC count (leukocytosis) and low levels of Hemoglobin and Hematocrit. c. Arterial Blood Gas reveal Metabolic Acidosis as the pH is low and low bicarbonate level. Pain Level: Using Pain Scale, Patient X rated his pain 9 out of 10. Vital Signs: BP= 90/50 PR= 128 bpm RR= 28 bpm SPO2= 95% PATHOPHYSIOLOGY NURSING CARE PLAN Acute Pain Imbalance Fluid Volume Risk for Infection DRUG STUDY Pip Taz Omeprazole Morphine Ranitidine CONCLUSION AND REFLECTION VI. Nursing Care Plan (NCP) a. List of problems b. Prioritized problems c. NCP (2 actual, 1 risk)