lOMoARcPSD|28697339
(Guided Reading Key: shorturl.at/inQRY)
● Cranial bones not fully ossified so allows for brain growth but inc risk brain/spinal cord injury
● Posterior fontanel closes at 2-4 months / Anterior fontanel closes by 12-18 months
● Skull/brain grow fast in early childhood so higher brain/spinal cord injury risk; head/chest circumference
equal at 2 yrs so biggest fall risk is under 2 yrs
Neuro
Assmt: Increased ICP pathophysiology - Intracranial Pressure Nursing Care NCLEX RN LPN
● LOC: Most important indicator of neuro dysfunction
○ Inc ICP -> Give IV osmotic diuretic (Mannitol), keep HOB @ 30 degree angle
○ Glasgow Coma Scale: Scale for responsiveness; Under 8 then intubate!
■ Max = 15: indicates best neuro fxn; Minimum = 3: total neuro unresponsiveness
● Conscious = Receptive to stimuli & Alertness = Arousal/ability to react
Timing of Signs
Signs of Inc ICP
Early Signs
● HA
● Visual disturbances (diplopia)
● N&V
● Dizziness or vertigo
● Slight change in VS
● Pupils not as reactive or equal
● Sunsetting eyes (iris appears to set into lower eyelid leaving sclera visible above iris)
● Slight change in LOC, restlessness
High pitched cry = Early sign of inc ICP in an infant
Infant has above signs plus:
●
●
●
●
●
●
●
Irritability
Bulging fontanelles
Wide sutures, inc head circumference (FOC)
Dilated scalp veins
High-pitched, catlike cry
9-10 glasgow coma scale
Some dec in LOC
Late Signs
●
●
●
Significant dec in LOC
Seizures
Cushing Triad:
○ HTN (inc systolic w/ wide pulse pressure; big gap between S&D)
○ Bradycardia
○ Irregular respirations
Fixed dilated pupils- brainstem herniation from inc icp
Posturing:
○ Flexor (Decorticate): Rigid flexion from lesions above brainstem in
corticospinal tracts, protect core
○ Extensor (Decerebrate): More severe; Rigid extension from brainstem
lesions, wrists/feet rotated out, not protecting core anymore
●
●
Traumatic Brain Injuries: Falls are a major cause till 12 y/o (13-17 is assault/sports)
● Safety gates at top & bottom of stairs to prevent falls
● Primary Injury = Hit by baseball
Secondary Injury = Swelling over time
Hypoxic-Ischemic Brain Injury (Submersion/Drowning):
● 5-10 min & resuscitated at scene: Few sx, full recovery w/o neuro impaired; may do hospital stay to
monitor F&E but overall no long term issues
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
> 10 min before BLS or pulseless > 25 min = poor prognosis
○ Cerebral edema
● Prevention = Key! don’t leave alone near bathtubs/water, keep buckets empty, drain covers
Seizures: Maintain airway: Don’t put anything in mouth! Roll to side if vomiting or inc secretions
● Safety: Bed low, remove items from area/body, rails up & padded on admission if seizure hx
● Admin meds, emotional support, education (triggers, pt/family teaching), bed rolls
○ Triggers can be hormonal (periods), med changes
● Absence Seizures: Sudden cessation of motor activity/speech w/ blank facial expression, eye blinking, or
mouth twitching, lasts less than 30 seconds & pt appears “spaced out”
● Prolonged: Over 5 min
● Status Epilepticus: Acute seizure over 5 min despite intervention or seizure clusters w/o full recovery
● Priority = Admin rescue benzo if seizure over 5 min
○ Rectal Valium/Diazepam (Diastat, pre lubricated)
● Electrolytes, gluc, blood gasses, temp, & BP monitoring if seizure over 15 min
● Nurses need to admin meds as ordered (benzos, antiepileptics), collaborative care
Meningitis: Inflammation of meninges covering brain & spinal cord
● PMH: URI sx x 1 week, +Brudzinski sign
● Presentation: Photophobia, HA 8/10 after medication
● Interventions: Dark env, low stimulation, seizure and isolation precautions
● Meds:
○ IVF
○ IV abx
○ Vasopressors (septic shock)
●
Bacterial Meningitis
Viral Meningitis
More virulent than viral
● Can be fatal- infants at greatest risk
Sx same as bacterial, but kid doesn’t seem quiet as ill
May be secondary to other bacterial infxs (otitis media, sinusitis)
Kid is automatically tx w/ abx on an emergency basis until bacterial
meningitis can be ruled out
Opisthotonic position w/ neck & head hyperextended to relieve discomfort
Full recovery, self-limiting; tx aimed at reducing sx
Droplet precautions
Allow position of comfort, acetaminophen to treat pain/fever, room shld
be dim & dec stimulation, monitor for seizures even tho rare
Reye Syndrome: Combo of recent viral infx & aspirin
● Acute Encephalopathy: Cerebral edema, neuro & liver dysfxn (high ammonia lvl)- progression to coma, loss
of DTRs, & cardiac/resp arrest (high mortality rate)
○ PMH: Influenza 1 wk ago. Aspirin given for fever & body aches
○ Presentation:
■ Photophobia
■ Sleepy/irritable
■ Itching
○ Interventions: Dark env, Low stimulation, Seizure precautions
○ Meds:
■ IVF
■ Corticosteroids
■ Vit K (sick liver-help w/ coagulation)
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
■ Glucose (r/t dec glucose production in liver)
Sx: Depend on causative organism
○ Fever (or sx of resolving viral illness)
○ Irritability
○ HA if old enough to tell u (toddler will be crying & fussy)
○ Bulging fontanelle (infants & young kids whose haven’t closed yet)
○ Alt mental status
○ Paralysis
○ Possible Kernig or Brudzinski sign (can see w/ meningitis as well)
○ Generalized weakness
● Tx: ICU support care; prevent secondary cerebral edema & metabolic injury r/t ammonia
& short chain fatty acid lvls; intubate/ventilate once comatose
● Prevention: Don’t give aspirin for flu-like sx, cold, chicken-pox/varicella
○ Give ibuprofen (have to be 6 mo+ for ibuprofen) or acetaminophen
(processed by kidneys not the liver)
● Decorticate posture seen in less adv stage of reye & indicates that condition improving
(progressing from decerebrate to decorticate posturing indicates improvement in
condition)
○ Decorticate Posture = Inflammation above brainstem
○ Decerebrate Posture = Inflammation in brainstem
Spina Bifida (Meningomyelocele): Chronic common neural tube defect; lumbosacral defect closed at birth
● Dec risk of NTD (neural tube defects): Folic acid 400 mcg/day for all women child-bearing age
● Defect in 1 or more vertebrae allows spinal cord to protrude at lumbar or sacral portion
● Impaired Physical Mobility: R/t neuromuscular impairment
● Impaired Urinary/GI Elimination: R/t sensory impairment (neurogenic bladder/bowel)
● Risk for Impaired Skin Integrity: R/t motor & sensory deficits, unable to tell hot or cold
● Risk for Latex Allergy Response: R/t multiple surgical procedures (no bananas, balloons, plant, gloves
[need latex free gloves] )
● Pre-Op: Dx before birth; transfer to speciality center/NICU until surgery
○ Monitor sac for leakage of CSF, Assess extremities for deformities, worry for meningitis
○ Frequently assess VS & sx of infx
○ Biggest issue pre-op = meningitis
● Post-Op: Manage infant’s post-op pain, Assess I&O, emotional support + education
○ Measure head circumference daily- biggest issue post-op = hydrocephalus
○ Place infant in primarily prone or side-lying position sleep
○ Keep diaper away from incision site
○ Assess for infx, motor deficits, & bladder/bowel involvement
○ Perform urinary catheterization regularly only if needed
○ ROM exercises as soon as possible
● Health Promotion of Spina Bifida:
○ Provide all recommended immunizations & routine screening
■ If child has seizure disorder, alert parents of seizure risk after immunizations
■ Screen for scoliosis annually starting at birth
○ Obtain urinalysis w/ culture in newborn period & when sx of infx noted
●
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
○
○
○
○
●
G&D Surveillance: Monitor growth (length/ht, weight, head circumference)
■ Monitor head circumference growth carefully because of hydrocephalus risk
■ Assess development status regularly. Motor skills delayed, can get scoliosis, cognitive defects
■ Enroll in early intervention program to promote development
■ Promote gradual independence in mobility/self-care
Nutrition:
■ Teach family correct cal intake/portions at each age to dec obesity risk b/c can’t move as much
■ Give guidance about inc fluids & fiber in diet to dec risk for constipation & UTIs
■ Alert parents that allergies to foods like bananas, avocados, papaya, kiwi, etc may occur b/c risk
of latex allergy
Elimination:
■ Teach family clean intermittent catheterization on regular schedule
■ Teach kid to do self-catheterization & care for catheter in prep for school entry
■ Teach families to initiate bowel training so bowel regimen established b/c lack of innervation
to anal sphincter predisposes child to being incontinent
Sleep & Rest
■ Position kid to prevent contractures & change position at night to dec pressure over skin
surfaces
■ Teach parents to be alert for apnea spells/snoring r/t Chiari Type II Malformation (part of
brain protrudes thru hole in skull)
Meds:
○ Stool softener
○ Glycerin suppositories
● Relations: Promote peer interaction, alert of psychosocial adjustment issues
● W/ any chronic illness: goal is independence/self-care
Hydrocephalus: W/ or w/o meningomyelocele
● Clinical Findings:
○ Infants: Inc FOC, split cranial sutures; high-pitched cry (can occur w/ any neuro issue); bulging
fontanel(s); irritability when awake; seizures
○ Toddlers/Older Kids: Setting-sun eyes; papilledema (optic nerve swelling); seizures; irritability; dec
LOC (later sx after irritability); inc BP; widening pulse pressure (cushing's triad)
○ Older Child: Unbalanced & uncoordinated
○ All Kids: Vomiting; lethargy; Cheyne-Stokes respirations
● Meds: Dec CSF (temporary measure; only helps slow progression)
○ Acetazolamide, Isosorbide, Furosemide; -ide
● Going to need shunt - ventricles -> peritoneum or atrium (VP or VA)
● Mgmt/Teaching: Assess all infants for hydrocephalus: Measure head circumference regularly & compare
to growth curve; Note any inc ICP sx (monitor for in pre-op)
● Post-op:
○ Place flat & on nonoperative side (off shunt)
○ If held, don’t allow head to be elevated
○ Monitor of infx sx & notify MD of:
■ Fever; LOC change; red incision site/along shunt tract; inc WBC w/ leukocytes or left shift
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Teach sx of Shunt Malfunction: Emesis, fever, vision/neuro changes, seizures, poor feed, red along
shunt system, HA
Cerebral Palsy: Most common chronic disorder & cause of disabilities in kids
● PMH: Delivery at 32 wks; Head lag at 6 mo
● Permanent mvmt/posture disorders; tense
muscles, uncoordinated impaired rigid
fine/gross motor activity; 1 or both sides of
body; Non-progressive
● Additional sensory, cognition,
communication, and behavior problems
● Spastic: Most common type; musc
stiff/tight; limited mvmt; mild to severe
○ Orthotics to assist w/ mobility
○ Thickened liquids to dec aspiration
risk
○ Spasticity of musc incs caloric need
so don’t restrict calories
○ Prolonged bed rest causes
contractures
● Clinical Presentation: Hypotonia (Dec muscle tone, floppy, limp, flaccid), head lag (concerned for kids over
4 mo who still have head lag), underweight, shld not be tip toe walking after age 5
○
○
○
Ataxic gait
Contractures
Dysphagia
○
● Meds:
○ Seizure Disorders: Antiepileptics, Benzos
○ Athetoid: Anticholinergics to dec abnormal mvmts
○ Spasticity:
■ Oral: Baclofen (skeletal musc relaxant), Dantrolene Sodium, Diazepam
■ Parenteral: Baclofen & Botulin Toxins
■ Intrathecal: Implanted Baclofen Pump
● Multidisciplinary Care:
○ Orthopedic Surgeon care, PT/OT: Spasticity causes deformities & contractures
○ Speech Therapy/Dietician: Communication, feeding difficulties (swallowing), many
need extra feeds
○ High-Cal supplements
Muscular Dystrophies: Progressive musc degeneration/wasting, weakness/hypotonia (early sx),
life-threatening
● Duchenne Muscular Dystrophy (DMD): X-linked Recessive (mother is carrier)
● PMH: Met milestones till 3 yrs, tripping, “Used to run faster than sister, but now slower”
○ Waddling gait; lordosis; difficulty climbing stairs, running, or pedaling bike
○ Gower’s Sign: Since leg musc weak, maneuver to raise self to standing
position w/ arms/legs then push off floor & rests 1 hand on knee. Pushes self
upright
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Pseudohypertrophy: Large calf muscles (fat musc not true muscle but looks muscular
-> knees may bend back)
○ Obstructive Sleep Apnea -> BiPap/CPAP
● Only women carry but the males are affected
● Muscular Dystrophies: Nursing Mgmt
○ Meds:
■ Cardiac: Beta blockers, ACE inhibitors
■ Corticosteroids: Slows progression
■ Ca supplements: Prevents osteoporosis
■ Antidepressants
○ Maintain body systems, safety, resp/kid/family support, max independence, assess
for/tx infxs, periop care when surgery required, suggest exercises that limit use of
excess musc/prevent fatigue (ex: ROM), high risk for obesity b/c in wheelchair
○ Late teens & early 20’s becomes fatal, may need surgery over time
Guillain-Barre: Ascending paralysis; Report inc hoarseness
■
Endocrine
Definition
S&S
CH: Endocrine
Hypopituitarism
Congenital
Hypothyroidism
Congenital Adrenal
Hyperplasia
Turner Syndrome
Klinefelter Syndrome
Low pituitary hormone
secretion lead to retarded
growth, gonadotropin and
thyroid/adrenal deficiency,
depend on which hormones
deficient.
Dec in T3, T4 slows
metab rate.
Embryonic
autosomal recessive
defect in thyroid
Gene conditions affect
adrenal glands;
interfere w/ normal
G&D of genitals d/t
dec or absent cortisol
synthesis; autosomal
recessive
Chromosomal
disorders interfering
w/ normal growth;
absence of X
chromosomes: 45 XO
karyotype; only in
females
Chromosomal disorders
interfere w/ normal
growth; excess X
chromosomes: 47 XXY
karyotype; only in
males
●
●
●
●
●
●
Short stature
Delayed bone age
Infertility
Intolerance to cold
Fatigue
Loss of hair
●
●
●
●
●
●
●
●
●
●
Pallor
Dec temp
Hypoactivity
(sluggish)
Dec musc tone
& reflexes;
hypotonia
Large tongue
Bradycardia
Constipation
Feeding
difficulties
Dry & cracked
skin
Edema at eyelids
●
●
●
●
●
Salt wasting - can
be life threatening
(shock)
Hyponatremia
Hyperkalemia
Hypoglycemia
Ambiguous
genitalia
●
●
●
●
●
●
●
●
●
●
Edema hands/feet
Low posterior
hairline/webbed
neck (extra skin)
Short stature
Delayed puberty
Amenorrhea
Normal growth till
3 yrs, then no
growth spurts
Infertile
Kidney, thyroid,
heart issues,
congenital heart
defects
Learning
difficulties/dec IQ
Small jaw, hearing
loss, low set ears,
osteoporosis
Downloaded by Katherine Mills (millskatherine37@gmail.com)
●
●
●
●
●
●
●
●
Not detected till
puberty
Varying degrees of
mental impairment
Severity of
intellectual disability
incs w/ additional #
of X chromosomes
Tall
Hypogenitalism
Gynecomastia
Sterile
Poor social
interactions
lOMoARcPSD|28697339
Tx
Replace growth hormone
every day till growth plates
close (SE: inc blood
glucose &
gynecomastia)
Thyroid hormone
replacement
Steroid
(hydrocortisone +/fludrocortisone)
replace (low cortisol
-> hyponatremia)
Growth hormone
Estrogen (beginning
around 12-13 yrs)
Testosterone
replacement starting at
puberty
Salt replacement
Nursing
Implicatio
ns
Kids reach normal adult
height, but more slow than
others (takes 3-6 months to
see changes)
Wear medical ID bracelet
Give med empty
stomach 30 min
before food
Inc steroid in times of
illness, injury and
stress
Separate from iron
& Ca supplements
by 4 hrs
Foster bond btwn
parent & child
Test at newborn
screening
Educate on learning
abilities and fertility
Invitro fertilization can
be effective
Teach parents
reconstructive surgery
options
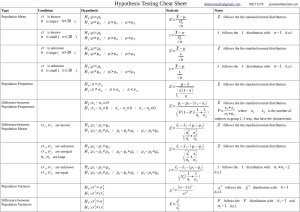
Insulin Types
Type
Rapid acting
Names
Onset
Humalog (Lispro), Glulisine,
Aspart
Afrezza
Short acting
Regular, Novolin
Peak
Duration
15-30 min
30-90 min
< 5 hours
<15 min**
10-20 min**
2-3 hours**
30-60 min
2-5 hours
4-12 hours
*Regular is the only one that
can be mixed with others and
only one that can be given
IV
Downloaded by Katherine Mills (millskatherine37@gmail.com)
Therapies (OT, PT,
speech)
lOMoARcPSD|28697339
Intermediate
NPH
1-2 hours
6-10 hrs
14-24 hours
Long acting
Glargine
3-6 hours
Minimal
24 hours
Detemir
3-4 hours
3-9 hours
24 hours
Degludec
1 hour
9 hours
42 hours
*During sickness: Need tighter gluc control, check for ketones in urine every 4 hours, blood sugar 2-3 hrs
*If not sick: Before meals
Special Considerations
Implications
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Puberty Insulin resistance & fluctuations in gluc
lvls
Insulin doses may need to inc b/c flunctuations
Developmental Approaches – Toddlers
Introduce parents to other families with children with diabetes or find support group.
Offer toddler choices of snacks & injection sites; offer finger foods
Developmental Approaches – Pre-School
Let kid help choose foods, let them wipe skin for shots and gluc checks
Needle play with dolls (w/ supervision); Play games to teach about hypoglycemia
Developmental Approaches – Elementary
Play board/computer games about diabetes, diabetes camps. follow diet, help w/ mgmt with supervision.
Help w/ meal plan/prep. Can count carbs, admin or begin assisting w/ insulin admin (drawing up &
injecting); do fingersticks w/ supervision.
Doesn’t fully comprehend how doing something now affects long-term (good diabetes control prevents
complications later)
If kid has electronic devices (phone, tablet, etc.), can download & use diabetes and carb monitoring apps
Developmental Approaches – Young
Adolescents
Support groups, negotiate plans to allow increasing responsibility for management w/ supervision
If child has electronic devices; download diabetes management apps
Impulsiveness, mood swings, struggle for independence and body image are key influencing factors and
can lead to noncompliance: care contracts used to foster accountability and inc compliance
Depression screen, test gluc before driving, sex education/protection
Developmental Approaches – Older
Adolescents
Shld begin independent w/ care by 16 years. May still need help w/ insulin dosing decisions.
Phenylketonuria (PKU): Autosomal recessive disorder of metabolism affects bodys ability to use protein
Must be detected early (screened in newborn), if untreated -> brain damage, development delay; autism-like behaviors
Fruits & veggies good, Lofenalac formula, carbs, low protein diet, spinach salad w/ mushrooms, fruit smoothie,
○ Avoid aspartame (artificial sweeteners such as coke), have diet low in phenylalanine
Precocious Puberty: When body begins puberty too soon; considered before age 8 in girls and age 9 in boys.
●
●
●
Admin hormone to stop puberty until they reach appropriate puberty time
MSK
Care Issues
Legg-Calve Perthes
Slipped Capital
Femoral Epiphysis
(SCFE)
Developmental
Dysplasia of the Hip
(DDH)
Osteomalacia
(Rickets)
Downloaded by Katherine Mills (millskatherine37@gmail.com)
Scoliosis
lOMoARcPSD|28697339
Definition
Blood supply to
femoral head
disrupted ->
avascular necrosis.
Ball of femur
(capital epiphysis)
slips off growth
plate
Femoral head
flattened & slowly
replaced w/ new
bone
Medical
emergency b/c
further slippage can
cause deformity or
necrosis
S&S
Limping/groin
pain, knee pain, c/o
after activity
Tx
Before 6 yrs:
Restrict movement,
casting
Abnormal relation
btwn ball & socket of
hip joint which there’s
inadequate coverage of
ball by socket or
dislocation of ball
from socket
Softening of bones
d/t lack of vit D or
inability to regulate
Ca & Phos
Sideways curvature & spine
rotation makes spine look like
"S" & 1 shoulder looks higher
than other.
Limping, thigh or
knee pain
Hip clunk, limited
mvmt, different leg
lengths, waddle, skin
fold
Bone fractures,
muscle weakness,
numbness, spasms
Asymmetrical hips &
shoulders, when bending at
waist = curvature & rib hump
Surgery
Pavlik harness (if < 6
months)
Vit D, Ca, Phos
Observation, bracing, surgery
Factors that reduce
formation of Vit D
Pain control, log roll (don’t
want spine bending/twisting),
neurovasc checks (perfusion,
skin color, cap refill,
sensation, AND mvmt)
Surgery (w/ or w/o
traction first)
After 8 yrs
(general): Surgery
Nursing
Implication
s
Care Issue
Couch potatoes (do
bedrest), pain
management
(NSAIDs)
Bedrest, stay off
affected side,
wheelchair, no
crutches unless keep
wt off affected leg
such as 12 y/o but
don’t use walker
Osteogenesis Imperfecta
Pavlik harness 24
hrs/day (can take off
for 1 hr to bathe quick,
daily skin check,
shirt/socks under
harness to protect skin)
↓ sun exposure, dark
skin, smog, ↓ milk
intake
Casting (spica cast):
nothing near entrance
of cast (no lotions)
Osteomyelitis
Juvenile Idiopathic Arthritis
Definition
Genetic defect impairs body's ability to
make strong bones -> easily fractured
bones; mistaken for child abuse
Bone infx & soft tissue
around bone
Autoimmune chronic disease resulting in joint
pain & swelling
S&S
Weak bones, bone deformities, brittle
teeth, blue sclera
Fever, chills, local swelling,
redness, warmth, knee pain
Swollen, red, painful joints, joint stiffness w/
limited mvmt, intermittent rash w/ fever, limp
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Bisphosphonate
Tx
Bracing, Surgery to place rods in long
bones for stability
Nursing
Implications
●
●
●
Don’t lift under armpits, no BP, no wt
bearing/contact activities; aware of child
abuse implications w/ multiple broken
bones (good assmt)
Long term IV abx for 4-6
weeks = major intervention
(ex: Vanco IV every 8 hrs)
NSAIDs, steroids, DMARDs (anti-arthritis),
(anti-inflammatory meds)
Erythrocyte sedimentation
rate (ESR) & C-reactive
protein = Indicators of
long-term infx/inflammation
Need to stay active w/ non-weight bearing
activities such as swimming, growth affected
Warm bath/shower to loosen up muscles/joints
helps w/ fxn + mobility
Implications of Fractures Growth Plate: Growth plates more likely to fracture but heal faster (improper healing can result
in growth abnormalities/bone deformities)
Red Flags r/t Fractures/Child Abuse: Fractures in under 6 mo, infant spiral fractures, multiple fractures any ages,
rib/sternal/vertebral fractures, depressed skull fractures
Nursing Implications Cast Care: Assess 5 P’s (pain, pallor, pulselessness, paresthesia, paralysis) circulatory check,
elevate, ice, not compression, odor, allow to dry, nothing stuck in cast, if itchy use dryer on cool setting, no heat to cast,
cover rough edges w/ moleskin, position changes. Compartment syndrome: pain greater than expected or w/ passive
mvmt
○ Primary intervention to dec cast swelling is elevation & then contact HCP (compartment syndrome)
Hematology: Hematologic system includes blood & bone marrow
● Affects & regulates (directly or indirectly) every body system; disorders benign or malignant
● Blood Components: Cellular Elements (RBC, WBC, platelets), Plasma
Iron Deficiency Anemia: Low RBC/Hgb d/t low iron from blood loss, nutrition issue, inc physiologic demand (rapid growth)
● Risk Factors: Breastfed infants, kids who drink excess cow milk, adolescents
● S&S:
○ Pallor
○ Pica
○ Fatigue
○ Irritability
○ Tachycardia
○ Tachypnea
● Tx:
○ Oral Iron Sulfate: May be hard to admin d/t palatability, absorb best w/ vit C
■ May be hard to admin d/t palatability
■ Take w/ vit C for absorption
■ Take on empty stomach unless GI upset
■ SE: Dark tarry/black stools, GI upset, constipation
■ Liquid shld be squirted in back of mouth -> blackens and stains teeth/clothes so teach to rinse or brush after!
○ IV iron
● Prevention:
○ Iron supplement for breastfed infants/preemies & iron containing infant formula
○ Screen from 12 mo to 5 yrs; screen adolescents
○ Iron rich foods: Shellfish, dark leafy greens, beans, dried fruit, red meat, quinoa
Issue
Sickle Cell Anemia
Hemophilia
Von Willebrand
Downloaded by Katherine Mills (millskatherine37@gmail.com)
Thalassemia
lOMoARcPSD|28697339
What is
it?
Hereditary autosomal recessive (1 abnormal
gene is carrier [sickle trait] & 2 abnormal
genes causes disease) abnormal hgb where
RBCs change shape & blood is viscous,
occludes vessels -> ischemia. (if both parents
have sickle cell trait, the likelihood that the
child will have the disease is 25%)
X-linked recessive bleeding
disorder; deficiency of
clotting factors.
Abnormal RBCs don’t carry O2 normally, they
stick tg and obstruct blood flow in capillaries
Hemophilia B (Christmas
Disease): Factor IX
deficiency
Impaired blood flow causes engorgement of
tissues, tissue ischemia
Hemophilia A: Factor VIII
deficiency “classic”
hemophilia
-Most women are carriers
and have 50% chance that
male offspring get
hemophilia; 50% chance
that female offspring will be
carriers
Degree of bleeding r/t
injury severity + clotting
factor amount
S&S
Triggers/
Precipitating Factors:
Dehydration, emotional stress, illness,
trauma (fever, infx, surgery), temp changes,
stress, hypoxia (change in altitude) -> RBCs
change shape in these situations
Bruising, bleeding to joints,
from circumcision,
nosebleeds, prolonged
mouth bleeding, oozing
from venipuncture or
finger/heel stick.
Complications: Pain, stroke, priapism, acute
chest syndrome, splenic sequestration, sepsis
(esp encapsulated organisms; ex: Strep
pneumo).
May be asymptomatic till
crawling/pulling to stand.
Bleeding Sites: Joint,
muscle, mouth, GI,
hematuria
Autosomal
dominant
bleeding disorder
lacks plasma
protein that
carries Factor
VIII.
Both
male/females.
Von Willebrand
factor helps
platelets fxn &
protects factor
VIII.
Autosomal recessive heme
disorder; Inherited blood
disorders of hgb synthesis
characterized by anemia.
[minor or major]
Mutation(s) in α- or β-globin
genes needed to synthesize
hgb.
Beta-thalassemia Major
(Cooley’s anemia): 2 mutated
genes w/ mod-severe sx;
needs chronic transfusions to
keep normal lvls.
IF mom has and
dad doesn’t
there is 50%
chance children
will be affected
Bruising easy,
Nosebleeds
(epistaxis),
Menorrhagia
Prolonged
bleeding w/
procedures
Pts w/ severe
phenotypes have
joint bleeding
similar to
hemophilia
-Joint Bleeding
(hemarthrosis) corresponds
w/ disease severity; chronic
arthropathy
-Factor lvls expressed as
percentage of activity
(100% in normal plasma)
-Mild (5-40%): Bleed from
trauma or surgery
-Moderate (1-5%): Bleed
from minor trauma, not
spontaneous
Downloaded by Katherine Mills (millskatherine37@gmail.com)
Pallor
Jaundice
Irritability
Stunted growth
Hepatosplenomegaly
lOMoARcPSD|28697339
-Severe (<1%): Frequent
bleeding episodes,
spontaneous
Tx
Hydration
Oxygen
Pain management
Prevention of pain crisis:
Stay hydrated at home.
Prevent of infx: Immunizations
(Pneumococcal, meningococcal). Penicillin
prophylaxis in young children.
Prevent stroke in those high risk: Chronic
transfusions
Prevnar decs invasive pneumococcal disease
(IPD)
Replace missing Factor – IV
(Factor VIII Recombinant:
Recombinate, Helixate,
Kogenate) (Factor IX
Recombinant: BeneFIX),
Plasma derived products
Tx based on
bleeding site,
target joint
status if
applicable & pt
age
Major bleeds correct w/
100% factor replacement &
minor w/ 50%
Tx is episodic or
prophylactic
Primary prophylaxis of
severe hemophilia = Reg
infusions VIII or IX; goal to
prevent joint bleeding
DDAVP (incs plasma VIII lvls)
for mild-mod
Standard/conventional tx is
chronic blood transfusions;
can cause iron build up and
need medications
Stem cell transplant is the
only cure
Nonreplacement:
DDAVP, Amicar
Replacement:
vWf-containing
Factor VIII
Hit head is
priority
Antifibrinolytic agents
(Amicar) for mucosal bleeds
Parents taught to do at
home.
For open wound after fall,
hold pressure for 15 min
Nursing
Implica
tions
Vaso-occlusive Crisis: Painful episodes,
Dactylitis (hands/feet) is 1st sx in older
infants
● Mgmt: Hydration, Oxygen, Pain control;
know Hgb and Spleen size baseline
Acute Splenic Sequestration: From
vaso-occlusion w/i spleen & splenic pooling
of RBCs; present w/ rapidly enlarging spleen,
marked dec in Hgb, abd pain/distention
● Tx w/ hydration & *caution* transfusion
○ Auto-transfusion: When transfused
RBCs cause spleen to release trapped
RBCs back to circulation
● May be hemodynamically unstable &
need intensive support
● Parents taught to check spleen size at
home
Aplastic Crisis: After viral infx (Parvovirus
B19), temp transient pure red cell aplasia;
severe Hb drop w/ low reticulocytes
For bleeding disorders:
Bleeding into joints (“target joints” = 3 bleeds
or more within 6 mo): limited mvmt, bone
changes/deformities
What to do when a bleed occurs:
Rest
Ice
Compression for at least 15 min
Elevation
*do RICE for joint bleeds
Educate: Admin factor, precautions. Avoid
high-impact sports/activities but do exercise.
Assess for joint pain, swelling, deformity.
Downloaded by Katherine Mills (millskatherine37@gmail.com)
Blood Product Support:
● Acute Issues:
○ Febrile Reaction
○ Allergic Reaction
○ TACO (fluid
overload)
○ Sepsis (rare)
○ TRALI
(transfusion-associat
ed acute lung injuryrare)
● Chronic: Iron overload
(Hemochromatosis):
Iron chelators to dec
iron build up associated
w/ multiple blood
transfusions
Iron Chelators for Iron
overload:
lOMoARcPSD|28697339
Chest Syndrome: Acute deterioration in resp
fxn; infx & asthma or no trigger
● Pulm infiltrate, fever, resp sx
● Tx: Abx, simple vs exchange transfusion,
supplemental O2, bronchodilators
Priapism: Prolonged painful erection that can
happen in kids, adolescents, adults
● Stuttering: Can be treated at home
● Severe: Over 4 hours; need emergency
care
● Hydration, urology consult, keep NPO in
case of aspiration/irrigation need, pain
mgmt
● If not treated, can result in impotence
Stroke: Cerebrovascular accident cause by
sickling process
● Transcranial Doppler (TCD) to screen for
stroke risk in kids
● Chronic transfusion therapy for primary or
secondary stroke prevention
● To stabilize pt and prevent further damage,
we rapidly reduce % of Hb S below 30%
thru exchange transfusion (priority)
● W/o screening & primary stroke
prevention risks are increased
● Stem cell transplant may be considered for
recurrent stroke
Fever/Sepsis: D/t chronic splenic infarcts,
most kids functionally asplenic by age 5 yrs
old
● Spleen is body’s main defense against
encapsulated organisms like Strep pneumo
● Infx w/ this bacteria can rapidly be fatalPneumococcal sepsis is lead cause of
death in kids w/ sickle cell disease
● Prompt abx therapy in any pt w/ sickle cell
disease can be lifesaving
● Prevention: Penicillin prophylaxis,
vaccination, EDUCATION
Cancer Treatment SE Mgmt/Prevention
Thrombocytopenia
Avoid NSAIDs
Keep invasive procedures to minimum when possible
May transfuse platelets before injections/procedures that are medically necessary
Avoid constipation
Oral care w/ soft bristle toothbrush, avoid dental floss & sharp/crunchy foods
Avoid activities that may cause injury
Educate re: home management of epistaxis
Nothing per rectum
Platelets < 20k are at highest risk for spontaneous or severe bleeding
Anemia
Transfuse when needed & Cluster activities to prevent/manage fatigue
Downloaded by Katherine Mills (millskatherine37@gmail.com)
Bind w/ iron in
bloodstream and allow
it to be excreted
● Deferoxamine SQ
infusion given at home
every night - ototoxic
● Deferasirox
*Nonadherence is common
issue w/ chelation therapy.
●
lOMoARcPSD|28697339
Neutropenia/Fever
Normal absolute
neutrophil (ANC) is >
1500
Mild: ANC 1000 to
<1500 Can amount
fever, have pus
Mod: ANC 500 to
<1000 Can mount
fever, have pus, may
look sicker if white
coat arises again after
being low
Severe: ANC < 500; no
white cells, may not
handle redness,
inflammation
Monitor closely for signs of infx
Avoid exposures (crowds, sick people)
Meticulous oral care
Cultures & antibiotics within 1 hr of fever! Don’t wait for cultures to come back; discontinue if cultures negative
● First priority is obtain blood culture/admin abx asap
● If appear ill/febrile/septic, fluid bolus shld also be started immediately and obtain blood
culture (can run at same time)
o REMEMBER “CPETC” and LOC are very important
PJP prophylaxis – Bactrim or pentamidine
Nothing per rectum
Avoid exposure to possible molds (playing in dirt, construction, fresh flowers or plants)
No live virus vaccines
Severe neutropenia places pts at risk for severe/overwhelming bacterial infxs that can progress to sepsis/death
quickly
Fever is an emergency in an oncology pt!
ANC Calculation: ANC = (%neutrophils + %bands) * WBC/ 100
Multiply TOTAL WBCs by [percentage of neutrophils {plus bands, if present} ÷ by 100]
●
Most times WBC is reported as “thousands per mcL” so in this example, 4.0 is actually 4,000
The WBC Differential: The different types of WBCs are reports PERCENTAGES of total WBC, and shld add up to 100%
●
Ex:
67.8% neutrophils
+ 0.8% bands (small neutrophils)
+ 17.4% lymphs
+ 11.6% monos
+ 1.6% eos
+ 0% basos
Mouth Sores
(Mucositis)
Meticulous oral care!
● “Salt & soda mouthwash” – warm water, baking soda, salt
● Alcohol-free mouthwash like Biotene or Nystatin oral wash 3 times a day to prevent thrush
Offer soft, room temperature, and cool foods
Avoid food/drinks that can irritate mouth, no spicy diet or crunchy/sharp foods b/c hard to eat
Mix food with butter, gravy, or sauce to soften it and make it easier to swallow
Pain medication as needed (and prior to eating)
Offer straw for drinking liquids
IVF if unable to drink
Consider nutritional support
Cannot scrape thrush off
Risk Factors: Steroids, poor oral hygiene, suppressed immune system
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
NV
Meds to prevent NV are given before chemo (ex: Ondansetron)
Need rx before discharge for PRN nausea medications.
Anticipatory NV: Can use ondansetron or low-dose oral lorazepam.
Instructions for families: When to notify the HCP/seek medical attention while receiving cancer tx
Temp > 38
Any bleeding (nosebleeds, bloody stools or urine, petechiae, bruising)
Pain or discomfort with urination or stool
Mouth sores
Vomiting or diarrhea
Persistent pain anywhere
Signs of infection (cough, fever, runny nose, tugging at ears)
Signs of infection at central line (redness, drainage, tenderness)
Exposure to communicable disease, esp chickenpox (sometimes give VZIG for varicella post-exposure prophylaxis)
Tumor Lysis Syndrome:
Huge complication of peds
cancers which have high
proliferation rate & are
chemo-sensitive
Breakdown of malignant
cells release intracellular
components into
bloodstream
Large # of cells lyse in
short time, such as w/ start
of chemo
Manifestations
● Hyperuricemia ->
acute renal failure
-> worsening
electrolyte
disturbance
● Hyperkalemia ->
arrhythmias
● Hyperphosphatemia
-> Hypocalcemiaseizures, renal injury,
tetany, arrhythmias
Treatment
Aggressive hydration 2x
maintenance
Correct electrolyte imbalance
If uric acid normal or mildly inc:
Allopurinol (to prevent uric acid
production; inhibits enzyme that
converts xanthine to uric acid)
If uric acid inc/rising fast:
Rasburicase (converts uric acid
to allantoin so easily excreted)Drug contra if G6PD deficiency
Nursing Implications
1. Admin IVF as ordered
2. Strict I&O (measure every hr)
3. Frequent lab draws- every 6 hrs
4. Daily weight
5. Monitor urine specific gravity (< 1.010)
6. Monitor for
● Hematuria
● Flank pain
● Irregular heartbeat
● Signs of poor perfusion (CPETC)
● Muscle cramps, twitching, tingling,
Trousseau sign (carpopedal spasm)
● Seizures
Prevention of Tumor Lysis Syndrome:
● Anticipate: Know which pts likely to have it
○ Leukemias w/ high WBC, organomegaly, bulky lymphadenopathy
○ Other cancers w/ high proliferation rates such as non-Hodkin Burkitt lymphoma
● Prevention: HYDRATE!!!
○ IVFs at 2x maintenance
○ NO POTASSIUM IN THE IV FLUIDS
○ Allopurinol
○ Strict I&O to detect any dec in UO
Mgmt of Tumor Lysis Syndrome:
● Hyperuricemia: After giving Rasburicase, send blood samples for uric acid on ice
● Hyperkalemia:
○ Hydration
○ IV insulin & glucose
○ Inhaled Albuterol
○ Potassium-lowering agents
○ If severe, transfer to PICU, dialysis
● Hyperphosphatemia:
○ Hydration
○ Phosphate binders
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
●
○ Cautious tx of hypocalcemia
Never let anyone home with tumor lysis syndrome
Oncology Basics Oncology Jamboard
Normal Cell Growth: Orderly, balanced, many checkpoints/feedback mechanisms to ensure nothing goes wrong
○ Genes insides cells tell them when to start and stop growing
● Cancer: Starts w/ single cell which has genetic change (mutation) -> causes it to divide in uncontrolled fashion
● Cancer Cells:
○ Grow when they should not grow, much faster than healthy cells
○ Don’t die when they should and don’t fxn like normal cells
○ Infiltrate and damage health organs/tissues
○ Spread thru body via blood or lymphatics
○ Use nutrients and O2 that healthy tissues need
○ Can often hide from body’s immune system
Peds Cancers: Unlinked to lifestyle/env; often no cause; different types of cells than adults cancers and biologically different
Leukemias: Proliferation of abnormal blood cells; bone marrow makes immature blast cells that don’t fxn normal, can’t
make healthy cells; most are acute, chronic leukemias are uncommon in kids; cancers of early blood forming cells
○ S&S:
■ ↓ RBCs: Anemia - pallor, fatigue, HA, limp
■ Blasts in marrow cause bone pain/refusal to bear weight.
■ CNS involvement: HA, cranial nerve palsies. May not have overt sx
■ Purpura (necrotic spots indicating DIC and sepsis -> rapid response & HCP asap), petechiae
■ Fever from leukemia or infx
■ Cap refill 3-4 sec, pulses strong
○ Dx:
■ WBC in peripheral blood high, low, or normal; dec WBC: infx
■ Platelets ↓: bruising, bleeding, nose bleeds (plt less than 10 -> spontaneous bleeding)
■ Hemoglobin ↓
■ 2 cell lines abnormal is concerning.
■ Confirmed dx w/: Bone marrow aspirate/biopsy
○ Tx/Nursing Implications: Chemo phases; all pts get intrathecal chemo to prevent/tx CNS disease
○ Acute Lymphoblastic Leukemia (ALL): Pre-B ALL (B-lymphoblasts) / T-ALL (T-lymphoblasts)
■ ALL: Prognostic Factors: Low, standard, or high risk; tx protocol will vary based on this
● At time of diagnosis:
●
Favorable
Unfavorable
Age
1 to 10 years
< 1 year or > 10 years
Initial WBC count
< 50k
> 50k
CNS or testicular involvement
Absent
Present
Additional Factors:
○ Leukemia cytogenetics
○ Response to induction- complete remission is favorable
○ If not in remission by end of 3rd mo therapy, prognosis is very poor w/ chemo alone
● Overall, expect 80% of pts w/ ALL to be CURED
ALL: Multiple phases of tx
● Induction Phase: 1st month; aim to eliminate as many cells as possible, induce remission (where
can’t detect any cancer cells in bone marrow)
○ Multiple chemo meds given plus oral steroids, intrathecal chemo
● Pre-maintenance Phase: Chemo for 5-7 months
○ More intensive tx, given in hospital/clinical w/ some oral meds and injections at home
●
■
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
● Maintenance Phase: 2 to 3 years of mostly oral meds at home, clinic visits once/month
ALL: Tx of Sanctuary Sites
● CNS:
○ All pts get intrathecal chemo whether they had blasts in CSF at dx or not
○ Chemo does NOT penetrate BBB well, so give chemo into CSF to prevent leukemia
from proliferating there, or to treat leukemia that was there at dx
○ For kids w/ CNS involvement at dx, they get inc # of LPs w/ intrathecal chemo,
sometimes radiation
● Testes:
○ Testicular biopsy at end of induction to see if any active leukemia
○ If there is, testicular radiation will be part of tx plan
Acute Myeloid Leukemia (AML): 4-5 cycles of very intensive chemo all given in hospital, pts stay
admitted for weeks after each course to be monitored for infx
■ All pts get intrathecal chemo, extra doses given for CNS+ involvement
■ Leukemia cytogenetics and response to chemo determine prognosis
■ Some pts may need stem cell transplant
■ Around 35% of pts w/ AML will relapse
Mixed phenotype acute leukemia (MPAL) has characteristics of both lymphoid and myeloid leukemia
Marrow is packed full of abnormal cells, crowding out healthy blood cells
Presentation:
■ Cytopenias:
● Pallor, fatigue, dizziness, HA
● Bleeding, excess bruising, petechiae (does not blanch when pressed on; oral petechiae, wet
purpose means low plts)
■ Bone pain in back, legs, and joints causing difficulty standing or walking
■ Fever
■ Enlarged liver or spleen
■ Mediastinal mass (T-cell)
■ Loss of appetite, wt loss
■ Night sweats
■ Sanctuary Sites:
● CNS sx may be present if CNS involvement
● Testicular enlargement if testes involved
Blood Counts:
■ Blasts may spill into peripheral blood and be seen on CBC differential
■ Total WBC may be high, low, or normal
■ Hgb & Platelets decrease
■ 2 cell lines down or low Hb/platelets along w/ elevated WBC are very concerning
Dx: Confirm dx by getting sample of bone marrow
■ Bone Marrow Aspirate: Needle placed into hip bone to remove liquid bone marrow
■ Bone Marrow Biopsy: Larger-bore needle removes small core of marrow
Leukemia Workup/Staging:
■ Lumbar Puncture: Done all all pts to determine CNS involvement & how much chemo they need
● Chemo given into spinal fluid at same time (intrathecal)
■ CXR to eval for mediastinal mass (before any anesthesia or sedation given)
■ Testicular exam in boys
Childhood Leukemia Risk Factors:
■ Down Syndrome
■
○
○
○
○
○
○
○
○
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
■ Li-Fraumeni (familial cancer predisposition syndrome-rare)
■ Prior hx of ionizing radiation
■ Prior hx of chemotherapy
Brain Tumors: Most common solid tumors in kids of brain & CNS; hx of cranial radiation is risk factor
○ Varies on are, type, how fast growing & extent of tumor:
■ Sx of inc ICP
■ Focal, localizing neuro sx
■ Gait/coordination changes
■ Vision or hearing changes
■ Cognitive or behavioral changes; speech issues
■ Failure to thrive
■ Fast-growing tumors have more abrupt s/s than slow-growing tumors
○ Dx: MRI = Gold standard for imaging; includes brain and spine
■ Biopsy vs excision vs debulking when possible
● Debulking = Surgery that doesn’t removal all of tumor but removes as much as safely possible
■ For some tumors, bone marrow is also evaluated to look for metastatic disease
○ Prognosis depends on: Tumor type, how fast it’s growing, location, age
■ Location (can it be surgically removed? Is it in the brain stem?)
■ Infants have worse prognosis
■ Younger children recover more of neuro deficits after surgery than older children
○ Tx of Brain Tumors:
■ Surgery: To gian tissue and remove/debulk tumors, or for hydrocephalus
■ Chemo: Used in some types, have to overcome BBB so high-dose regimens are often used for
aggressive tumors. Some chemo may be given intrathecally
■ Radiation: Used alone or combo w/ chemo to treat radio-sensitive tumors; try to avoid completely in
children < 3 yrs
Non-CNS Solid Tumors:
● Neuroblastoma: Smooth, hard, nontender solid tumor along sympathetic nervous system dx in young children (rare
after 5 yrs of age)
○ Malignancy of sympathetic nervous system
■ Common sites: adrenals, chest, abdomen, or pelvis
■ Spreads easily via lymphatic and can be widely metastatic at dx
■ If bone marrow involved, may have cytopenias
○ Sx: Pain, fever, malaise, wt loss, abd distention- they look and feel sick, Palpable abdominal mass that
crosses midline is concerning for neuroblastoma
○ Dx: CT/MRI & MIBG scan; Tumor and bone marrow biopsies
○ Prognosis & Staging: Prognosis depends on age, tumor traits/genetics, and amount of metastatic disease;
higher age and higher stage = worse prognosis
■ The more widespread the disease, and the older the child, the worse they do
■ BUT- there’s a unique phenomenon (stage MS) where infants < 18 mo old who have neuroblastoma
in skin, liver, bone, and bone marrow w/o high risk traits, can have spontaneous regression of disease
w/o tx
○ Tx of Neuroblastoma: Based on staging; chemo, radiation, surgery, autologous stem cell transplant
■ Immediate risk- Chemotherapy
■ High risk- High dose chemo w/ autologous stem cell rescue, radiation, and immunotherapy
●
Wilms Tumor: Most common renal tumor in children - also called nephroblastoma
○
Rapidly growing kidney tumor peak age 3-4 yrs
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Painless firm abdominal mass doesn’t cross midline, systemic sx not common, may have hematuria or
flank pain (lower back pain)
○ Often 1st detected by family in bath or on routine checkup by provider
○ Dx: Sono, CT. CXR
○ Friable, gelatinous capsule that may rupture and spill tumor cells thru abdomen & pelvis; safety alert:
DON’T palpate abdomen (tumor could rupture) place sign
○ Metastatic Sites: Lungs, rarely in both kidneys at dx, not usually metastatic, but multiple primary tumors
○ Tx: 1st is tumor resection done with nephrectomy then chemo
■ Not all pts require radiation
■ For bilateral renal involvement - biopsy 1st, then 6 wks chemo, then partial nephrectomy on less
involved side & full nephrectomy on more involved side before rest of chemo is given
Osteosarcoma: Most common bone tumor in children & adolescents; in long bones around knee joint
○ Peak incidence in rapid growth years (2nd decade of life starting w/ adolescent growth spurt)
○ Involves long bones (appendicular skeleton), most common sites are distal femur & proximal tibia
○ Dull, aching, constant pain worse at night
○ May or may not have soft tissue mass and swelling, altered gait
○ Some have pathologic fractures
○ Risk Factors:
■ Prior radiation (occurs btwn 4-40 yrs after radiation)
■ Li-Fraumeni syndrome
○ Most common metastatic site is lung
○ X-ray/MRI or CT of tumor, CXR (to lungs) to eval extent of disease
○ Tumor biopsy to confirm dx, then 3 mo of chemo
○ Definitive surgery - limb salvage, can be joint replacement. Alternative is rotationplasty, rarely amputation
○ Then additional chemo about 1 yr total
○ Prognostic Factors:
■ Presence of metastatic disease
■ Response: Percent tumor necrosis
○ Osteosarcoma is typically radioresistant (THINK: teens resist stuff and are stubborn)
○ Persistent dry cough for 1 week is concern-> went to lungs
○
●
●
Ewing Sarcoma: In bones/soft tissue around bones; school-age and teens
○
○
○
○
○
○
Axial or appendicular skeleton- can start from any bone & have pathologic fractures
Intermittent pain that worsens over time, worse w/ exercise and at night, swelling
10-20% present w/ systemic sx (fever, malaise, anorexia, wt loss, night sweats)
Can metastasize/spread to lungs, bone, bone marrow
Metastatic disease presence is most important prognostic factor. Pts w/ pelvic primary lesions tend to do
worse
X-ray/MRI or CT of tumor, CXR to eval extent of disease; Tx: Chemo, Radiation and/or surgery
Treatment: Protocol-based
●
Chemo: Prevents proliferation of cancer cells
○ Route: Oral, IV, SQ, IM, intrathecal
○ Timing is important
○ Indiscriminately attacks any rapidly dividing cells in body
■ Hair
■ GI Tract: Mucositis, NV, Pain
■ Bone Marrow: Bone Marrow Suppression, Cytopenias
○ Leukopenia, neutropenia -> Immunosuppression, poor wound healing
○ Anemia -> Fatigue, HA, Poor PO, Transfusions
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
○ Thrombocytopenia -> Bleeding, Bruising
○ Chemo-induced NV: Effects vomiting centers in brain; anticipatory NV
○ Malnutrition: Inability to take in enough cals b/c of NV, mucositis, fatigue
○ Long-term Effects: Body systems & neurocognitive effects, organ damage, secondary cancers
● Radiation: High energy particles/waves destroy cancer cells
○ Used in radiosensitive tumors, combo w/ chemo or surgery
○ Many long-term toxicities (worse in children under 5 yrs of age)
● Surgery:
○ Tumor Resection (fully removed)
○ Debulking (making tumor smaller)
○ May be used for staging
● New Therapies: Immunotherapy, Biotherapy, Targeted agents
Nursing Care of Child w/ Cancer:
● Safe chemo admin- port or external central line
● For infusion reactions, 1st priority = stop infusion!
● Prevent/tx of infx
● Maximize nutrition and hydration
● Manage pain, SE
● Education/discharge planning
● Monitor development
● Psychosocial assmt/support
● NOTHING RECTAL for any oncology pt b/c high risk INFX (no enema, no temp, no suppositories)
● Most common bone tumor metastasis is lungs
Past Comprehensive Content- G&D 8 questions
Communicating with Children.docx
Erikson and Piaget.docx
Milestone & O2 Quizlet: https://bit.ly/3CGsx60
Piaget's Theory of Cognitive Development
Infant: Birth to 1 year
Erikson’s Psychosocial Development: Trust v Mistrust (birth-1yr)
● Caregivers responding to Maslow’s basic needs develops trust
○ Involve parents, hold baby often
○ Provide comfort after painful procedures, meet food/hygiene needs
○ Get on eye level, encourage parents to room in, manage pain
Piaget’s Cognitive Development: Sensorimotor (birth- 2yr)
● Learn relationship btwn themselves and env. thru sensory, mvmt, & motor perceptions
○ Body language (calm), Soothing voice, Facial expressions
○ Crib mobiles, manipulative toys, wall murals, & bright colors for interesting
stimuli/comfort, Use toys to distract baby during procedures & assmts
○ Ex: Pt imitates brother; he smiles when brother smiles
Major Infant Stressors: Separation from parents (separation or stranger anxiety), Impaired trust
Key Points for Infants:
● Avoid abrupt mvmts; advance slowly
● Limit stranger presence
● PARENTS provide best source of COMFORT
● Best strategy to facilitate trust in infant is responding to basic needs
Toddler: (1-3 yrs)
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Erikson’s Psychosocial Development: Autonomy v Shame (1-3 yr)
● Develops independence and self-control; inc independence in many spheres of life
● Negativism: Toddler wants to do things themselves
○ Offering choices promotes autonomy in toddlers
○ Repetition/rituals, Get on eye level, Praise
○ Give a job to do (this gives them control/autonomy)
● Nursing Applications: Allow self-feeding opportunities, encourage kid to remove and put on own
clothes, brush teeth, or assist w/ hygiene.
○ If immobilization for procedure needed, proceed quickly, give explanations/comfort
Piaget’s Cognitive Development: Preoperational (2-7 yr)
● Differentiates self from others and objects, Experiments w/ behaviors
● Animism: Objects have characteristics, they can imitate and substitute in play
○ Repetition
○ Short concrete terms
○ No reasoning b/c unable to reason at this age
● Toddler (1-3 yrs) would be end of sensorimotor and beginning of preoperational
○ Shows inc curiosity & explorative behavior; language skills improve
○ Ensure safe surroundings to allow opportunities to manipulate objects; name objects & give
explanations
Major Toddler Stressors:
● Separation from family
● Loss of control
● Restriction of movement
Key Toddler Points:
● Signature phrase is “No!”
● Offer viable choices such as “do u want to take pink medicine or white medicine first?” NOT “do u
want to take ur medicine now or later?”
● Rituals are very important
● Use 5 senses to explain things (what it will look, sound, smell, feel, and taste like)
○ Limited concept of time so teach right before a procedure and emphasize when it will end
○ They are very literal so watch your words!!
Preschooler: 3 to 6 yrs
Erikson’s Psychosocial Development: Initiative v Guilt (3-6 yr)
● Likes to initiate activities, please others, eager to learn
● Initiates many activities but never finishes
● Feels a sense of accomplishment when successful ->>> self-confidence
○ Offer choices
○ Tell them how to cooperate
○ Let them handle equipment to lessen anxiety about strange objects
○ Assess concerns as expressed thru their drawings
○ Accept choices & expression of feelings
Piaget’s Cognitive Development: Preoperational (4-7 yr): Inc verbal but has limitations in thought
processes, causality often confused so they may feel responsible for causing an illness
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Egocentrism: Toddlers & preschoolers have self-centered understanding of world; can only see
from their perspective
● Transductive Reasoning: Create connection btwn 2 events that occur at same time even tho there’s
nothing in common
● Magical Thinking: They cause events to happen
● Imaginary Friends
● Conservation: Preschoolers don’t yet understand that changing form a substance doesn’t change
it’s amount, volume, or mass
● Offer explanations about all procedures & treatments; clearly explain that child is not responsible
for causing an illness in self or family member
● 1 category (ex: it’s cat or dog)
● Ex: When asked how old she is, pt showed 3 fingers & said “this many”
Major Preschooler Stressors:
● Mutilation
● Punishment: Magical thinking (they cause events to happen)
● Loss of competence (initiative)
Key Points:
● Modesty is important
● Signature phrase is “Why?”
School Age
Erikson’s Psychosocial Development: Industry v Inferiority (6-12 yr)
● Interested in how things work
● Initiates activities but now sees them thru
● Competence/mastery = Goal; kid gains sense of self-worth from involvement in activities
● Encourage to continue schoolwork while hospitalized, bring favorite pastimes to hospital; help
them adjust to limitations on favorite activities
● Inc interaction w/ peers
○ Reassure
○ Treat as person (don’t talk about them to their parent, talk to them)
○ 3rd person speech (“Some kids say this medicine tastes bad”)
Piaget’s Cognitive Development: Concrete Operations (7-11 yr)
● Child capable of mature thought when allowed to manipulate & see objects
● Able to view world from another point of view
● Can think thru actions
● No abstract thinking
● Collections: Classifies into different sets
● Conservation
○ Prepare for procedures
○ Simple, concrete terms
○ Be specific
● Give clear instructions about tx details; show them equipment that will be used in tx
● Multiple Categories:
○ Ex: when lady asks pt how to get to library, pt told her to turn to her right at the next hall
●
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Ex: After watching show about animals, pt tells mom that lions are extra big cats (big, cat
-> multiple categories referenced)
Major School Age Stressors
● Loss of competence
● Failure
● Forced dependence
Key School Age Points:
● Give them simple tasks and choices
● They want to be involved in their care
● Signature phrase is “How does this work?”
● Finds classifying into different sets and collecting things important
○
Adolescents: 12 to 18 yrs
Erikson’s Psychosocial Development: Identity v Role Confusion (11-20 yr)
● Developing own sense of self; leads to independence from parents & reliance on peers
● Believes other ppl are closely listening to and watching them
● Exploration of personal, professional, and societal roles (adult vs child)
● Provide separate recreation room for teens hospitalized; take health hx and perform exams w/o
parents present; introduce teen to other teens w/ same health problem
● Revisiting previous stages
● Interaction w/ peers is KEY
○ Privacy & confidentiality
○ Give respect and feedback
Piaget’s Cognitive Development: Formal Operations (11-20 yr)
● Abstract, mature, logical, organized thinking
○ Ex: Pt answers questions w/ hypothetical situation (Needs an unknown)
● Give clear, complete info on healthcare/tx, offer both written and verbal instructions, continue to
give education on disease to adolescent w/ chronic illness, as mature thought now leads to greater
understanding
● Thinks about problems from all views & can rank solutions
○ Ask what they know and start from there
○ Ease into discussions
○ Avoid detailed discussion; they still need simple explanations and will be afraid to ask for
clarification in fear of sounding dumb
○ Use assuming language such as “How many cigarettes do u smoke?” instead of “Do u
smoke?”
Major Adolescent Stressors:
● Being different from peers/threats to their physical state
● Lack of independence and privacy
● Being ignored as an individual (talking to the parent instead of to them)
Key Adolescent Points:
● #1 plan of care issue is noncompliance
● PEERS ARE KEY
● Discuss interests
● Primary concern is the present
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Signature phrase is “I know.”
Implementing care contract will help give sense of responsibility, control, & independence thats a
successful strategy for fostering compliance
G&D Peer Notes :
Growth and Development.docx
Developmental Milestones Vids:
Infant Developmental Milestones Mnemonic Pediatric Nursing NCLEX Review
●
PEDIATRIC MILESTONES MEMORY HACK - YouTube
●
Quizlet on stages + communication
● https://quizlet.com/717775860/ch-communication-flash-cards/?i=29fr6m&x=1jqY
“Most People Can Get This”
●
●
bÄ
M = Music/Mobiles (Infants)
P = Push/Pull/Pound toys (Toddler)
C = Colors, Coloring, Characteristics (Preschool)
G = Games (School Age)
T = Themselves (Adolescents)
Infants: By end of 1st yr, fully active in exploring world; crawling, creeping, or walking; enjoy dropping,
throwing, squeezing, and “making things happen”.
● Puppets, soft plushies, shape sorter, bath book, musical mobile, board book, texture dog, mirror
board book, soft stacking cube, crib mobile (pooh), busy ball, rattles, metallic mirror, cow book
Toddlers: Joy in experimenting w/ mvmt. Intense exploration of toys/objects & quality/adaptive use in play.
Piling up blocks + knocking them over is enjoyable. 1st pretend play is “as if” doing daily activities.
Pretend to sleep, eat, or bathe. Enjoy playing near each other (parallel play) but not likely to share
● Sorting cube, push lawnmower, bowling set, drum, large hand puppets, plastic pail and shove,
nesting cups, coloring book, wood puzzles, elmo potty time book
Preschoolers: Most playful; mvmt abilities continue to develop w/ refinement of manipulative activities.
Pretend or dramatize events w/ others. Sociodramatic play represents more roles, events, and object
substitution. Real & pretend aren’t firmly separated in younger preschoolers; therefore, they “become”
rather than “pretend to be”. Love to construct and build. Preoperational
● Dollhouse, small pieces, finger puppets in ziplock bag, blue soccer ball, small white soccer ball, 2
barbie dolls, abacus, doc mcstuffins medical kit, elmo kit, polly pocket house, cooking and dress up
supplies in plastic bag, doll, walkie talkies, cell phone, candy land board game
School-age: Play games w/ others rather than specific interest in toys; social time, develop elaborate themes
in sociodramatic play. Many themes represent blood/thunder melodramas. Games w/ rules &. Older
school-age kids turn more creative/inventive in arts/crafts & types of choices for play. Prefer to play w/
same-sex peers; enjoy “fooling around” w/ friends and sitting/talking w/ adults.
● Lite bright, goal in mind, tinker toys, 20 question challenge, frozen playing cards, monopoly,
regular playing cards, batman activity book, Ill-advised fun, word search book
Adolescents: “Play activities” almost all peer directed. Interests are reading, music, sports, or movies. This
is time when privacy is important. May not be interested in talking to adults they don’t know.
Examples of Play:
● Solitary: Engrossed in play; no interaction w/ others (ex: playing w/ toys alone)
○ Infants (0-12 months)
● Parallel: Mimics other kids play but doesn’t engage other kids (ex: playing in sandbox next to each
other)
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
●
●
●
●
○ Toddler (12 months- 3 years)
Associative: Very social w/ no rules (ex: playing “house” tg but not organized manner
○ Preschool (3-5 years old)
Cooperative: Concrete organization, some rules, and a goal, but child is out to win for themselves
(ex: “I win”, board games, candyland)
○ School age and adolescents (6-18 years old)
Collaborative: Kid’s work toward common goal through sharing (ex: “I win as a team”,
competitive team sports, soccer, debate team)
○ School age and adolescents (6-18 years old)
Medical: False medical equipment kids play w/ to alleviate fears about procedures (ex: child life
“dolls”) toddlers and up
Age
Gross Motor Skills
Fine Motor Skills
Language Skills
Toys
3 Months
Raises head 45
degrees from
prone
Holds hands in front
of face; hands open
Coos
Mobile; contrasting colors &
patterns; mirror; music; rattle
4-5 Months
Lifts head and
looks around;
rolls over; lifts
head 90 degrees
from prone
position; head lag
disappears
Bats at objects;
grasps rattles; holds
bottle & carries
objects to mouth;
primitive reflexes
disappear; reaches for
object w/ open hand
Laughs, raspberries,
vocalizes in response
to others; responds to
name
Fabric or board books;
easy-to-hold toys that make
noise; floating/squirting bath
toys; soft dolls or animals
6 Months
Tripod sits; rakes
objects; stranger
anxiety begins
(6-8 mo.)
Releases objects to
take another; rakes
objects
Squealing
8 Months
Sits unsupported
Gross (crude) pincer
grasp
Babbling; follows
simple commands
9 Months
Crawls
Bangs objects
together; drinks from
cup w/ assistance
10 Months
Pulls to stand;
cruises/stands
holding to
furniture
Fine pincer grasp;
puts objects into
container and takes
out; feed self w/
fingers; object
permanence
Gives meaning to
names; mama and
dada; recognizes
objects by name;
imitates animal sounds
12 Months
Sits from
standing; walks
independently
Feeds self w/ cup and
spoon; pokes w/
finger; holds crayon
and mark on paper;
babinski reflex
*2-4 months: posterior fontanelle
closes
*6 months: teeth begin erupting
*12-18 months: anterior
fontanelle closes
Uses 2-3 recognizable
words with meaning
Downloaded by Katherine Mills (millskatherine37@gmail.com)
Plastic cups, bowls; mirror;
building blocks; stacking toys;
busy boxes; balls; dolls; board
books; toy telephone;
push-pull toys (at 12 months)
lOMoARcPSD|28697339
negative (can’t walk
if it’s positive)
18 Months
Climbs stairs w/
assistance
Turns multiple book
pages; removes
shoes; stacks 4 cubes
Understands “no”;
uses 5-20 words;
knows 200 words;
sometimes answers
“what’s this?”
2 Years
Runs; kicks ball;
stand on tiptoe;
carries objects
while walking;
climbs w/o
assistance
Builds tower of 6 or
7 cubes; right or left
handed; scribbles;
turns knobs; puts
round pegs into holes
40-50 words; 2-3 word
sentences; points to
body parts & pictures;
uses my or mine
3 Years
Climbs; pedals
tricycle; walks up
and down stairs
w/ alternate feet
Undresses self;
copies circle; builds
tower of 9-10 cubes;
holds pencil in
writing position;
screws/unscrews lids;
turns book pages 1 at
a time
4 Years
Throws ball
overhand; kicks
ball forward;
hops on 1 foot;
stands on 1 foot 5
seconds; hops
and skips
Uses scissors well;
copies capital letters;
draws circle and
square; draws a
person w/ 4 body
parts
Tells stories;
understands same and
different; asks many
questions; knows at
least 1 color; can
count a few numbers
Jigsaw puzzles; creative
supplies (crayons, paint,
scissors, paint, glue); puppers,
dress-up clothes, props; play
kitchen and pretend food;
sandbox; dolls and accessories
5 Years
Skips;
somersaults; may
skate and swim
Prints some letters;
draws person w/ at
least 6 body parts;
dresses and undresses
w/o help; ties
shoelaces; uses fork,
spoon and knife with
supervision; copies
triangle; cares for
own toileing
Long, detailed
conversations; uses
past, future, and
imaginary; answers
questions using why
and when; can count
to 10; recalls parts of a
story; speech fully
intelligible &
grammatically correct;
says name/address;
tells creative stories
Swing sets; driving toys;
blocks, legos; simple board
games; dollhouse w/
accessories; imaginary
playmates common
*33 months: deciduous teeth
eruption complete - 20 teeth
Push-pull toys
Household items (plastic
bowls, cups, utensils, etc);
child-size household items
(kitchen, broom, etc); blocks;
dolls; cars; manipulative toys
with buttons, knobs; puzzles;
stacking toys; beads to string;
Understands
blocks; push-pull toys;
prepositions; follows 3 tricycle; music; chalk, paint,
part commands; half
crayons; buckets, shovel; bath
speech understood by
toys
ppl outside family; 3-4
word sentences; vocab
of 1,000 words; can
say name, age, and
gender; uses pronouns
and plurals
Object Permanence: 8-12 months
Chest circumference > head circumference: 2 yrs
Understands Conservation: 7 years
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Peer Group as Major Influence: 15 years
Past Comprehensive Content- Resp
5 questions; Peer Tutor Notes:
Respiratory (1).docx
Resp Anatomy/Physiology System of Kids:
●
●
●
●
●
●
●
●
●
●
●
Nasopharynx & nares smaller -> more prone to occlusion, harder to breathe esp. infants b/c they’re nose breathers
Small oral cavity; large tongue -> easily occluded
Long, floppy epiglottis -> prone to occlusion
Lymph tissue grows rapidly -> more prone to resp distress
Thyroid, cricoid, tracheal cartilages immature -> more prone to collapse unless able to compensate
Fewer musc functional in airway; harder to have active resistance & cough stuff up
Larynx & glottis higher in airway which makes it easier to have airway occluded/easier to choke
Chest wall more pliable, Chest round at birth
Ribs & diaphragm horizontal; abdominal breathing until 5-7 y/o & then thoracic breathing
Large amounts of soft tissue around airway -> more prone for inflammation & swelling can cause occlusion
B/c kids have smaller airways they already have inc airway resistance combined w/ dec chest excursion, therefore have
higher RR -> inc risk of swelling & infection, less likely to compensate
What Abnormal Breath Sounds Could Indicate
Stridor
Wheezing
Crackles
Rhonchi
Continuous high-pitch
crowing sound in inspiration
d/t partial obstruction of
larynx or trachea
High pitch continuous musical
sound d/t air passing thru an
obstructed, narrow airway; heard
during expiration
Alveolar rales; fine, short high
pitched intermittent d/t air
passing thru fluid, pus or
mucus heard in bases of lung
lobes during inspiration
Large airway sounds;
continuous
gurgling/bubbling heard
in inspiration and
exhalation
Foreign body, croup, swelling
in throat, abscess, or tumor,
laryngospasm
Asthma, chronic bronchitis,
emphysema, pneumonia, allergic
reaction, foreign body inhaled into
lung
Pneumonia
Pneumonia, cystic
fibrosis, chronic
bronchitis
Loud on anterior neck, as air
moves turbulently over
partially-obstructed upper
airway
Classic Wheeze = Sibilant Wheeze:
High pitched whistle like sound
Coarse Crackles: Low-pitched
and moist, heard in pulmonary
oedema and bronchitis
May clear with
coughing
Medication = Racemic
Epinephrine
Rhonchi: Sonorous wheeze (deep
low pitch rumble/coarse sound as air
go thru tracheal/bronchial passages
in presence of mucus/resp
secretions)
Fine Crackles: Like hair
rubbing near ear; heard in CHF
and pulmonary fibrosis
Pleural Rub: Mvmt of inflame pleural surfaces against 1 another in chest wall mvmt; harsh grating or creaking
● Causes: TB, pneumonia
● Heard in lower anterior lungs & lateral chest in both inspiration & expiration
Respiratory Arrest: Cessation of respiration (no longer breathing)
Resp Distress vs Failure (https://www.youtube.com/watch?v=XV2OrrQm0T0)
Resp Distress: Inc work of breathing WITH adequate gas
exchange (pt is compensating), still able to oxygenate tissues
Resp Failure: Inability to maintain adequate oxygenation;
compensatory mechanisms fail; no longer able to meet demands
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Airway is open; normal respiratory sounds possible or
abnormal
Airway obstruction possible (can;t get enough oxygen in/out) ;
can occur w/ or w/o resp. distress (usually w/o in poisoning)
S/S:
●
●
●
●
●
●
●
●
●
S/S:
●
●
●
●
●
●
●
Retractions
Diaphoresis
Use of accessory muscles
Grunting
Agitation
Tachycardia
Head bobbing
Pale
Position of comfort like tripod or wanting to sit up
rather than laying down
Moderate Resp Distress: “Panic look”
Severe Resp Distress: Nasal flaring, mouth open
Inc rate (tachypnea) = Inc work (inc resp effort)
Inadequate effort- can be resp depression from meds, or
getting too tired, paralysis d/t Cspine injury
●
●
●
●
●
●
Dec resp effort (progress to no resp effort)
Gasping
Stridor
See-saw breathing
Cyanosis (blue, purple, pale) -> check mucous
membranes, soles of feet, palms
Slow RR
Bradycardia
Dec LOC/change in mental status
Sleepiness
Can occur without distress (cause = resp depression)
Sats go down
Resp Failure = Most common pathway to cardiopulmonary arrest
in children
Management:
● Support compensatory efforts of child
○ Elevate HOB (do NOT lie down)
○ Allow pt to assume “position of comfort”
○ Minimie sources of stress- cluster care
○ Suction as needed (Yankaeuer/Neosucker)
○ Humidified O2 (not high flow)
○ Do NOT give oral feeds/fluids if RR > 60
■ NGT for abdominal distention
● Resp distress -> resp failure
○ Intubate/ventilate
● Try to calm pt to (1) dec oxygen demand & (2)
reduce fatigue (child working harder- gets tired, stops
breathing) (3) inc oxygen delivery - more effective
breaths
Red Flags (Progressing from reps distress to failure)
● Early:
○ Restless/Irritable
○ Tachypnea/Tachycardia
■ Infant/child w/ RR >60 at risk for apnea second to inc CO2 & inc WOB
○ Inc effort- retractions, nasal flaring, head bobbing, grunting
● Late:
○ Dec in RR or irregular pattern
○ Diminished breath sounds
○ Dec LOC (drowsiness)
○ Skin color (cyanosis)
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
○ Apnea/Bradycardia
● Pt may rapidly progress to resp failure
● Nursing Alert: The quieter the child, the greater the cause for concern!!!
○ If any of these signs occur, get medical help immediately!!
■ Inability to swallow
■ Absence of voice sounds
■ Inc resp distress
■ Acute onset of drooling (sx of supraglottic obstruction; can’t manage secretions)
Tripod Position: Open mouth, leaning forward; Don’t force child to lie flat
Oxygen Delivery Methods:
● “Blow-by”: Unreliable
● Nasal Cannula: ¼ to 4 L max
○ 5-8L would have to be heated/humidified high flow - Optiflow/Vapotherm
● Venturi Face Mask: 24-48% variable; most precise method of O2 admin
● Simple Face Mask: 6-10 L (40-60%)
● Non-rebreather Mask: 100%
● Bag-valve Mask (BVM) for apnea
● Bi-pap/CPAP
● Intubation/Mechanical Ventilation
Acid-Base Imbalances Made Easy in 5-minutes with Kendall Wyatt
Respiratory Acidosis & Alkalosis - Acid Base Balance - ABGs Nursing, NCLEX, RN & LPN
Metabolic Acidosis & Alkalosis I Acid Base Imbalances for Nursing NCLEX, RN & LPN
Acidosis vs. Alkalosis
Normal Value
pH
7.35-7.45
pCO2
HCO3
35-45
22-26
Common Cause
N/A
Dec
Respiratory Acidosis
High
Normal
CO2 retention: Drug OD, CNS trauma,
pneumonia, airway obstruction, asthma
attack
Low
Normal
Hyperventilation (anxiety, fever, pain)
Normal
Low
Diabetes, DKA, shock, renal/kidney
failure, diarrhea
Normal
High
Vomiting, diuretics, NGT suction
Inc
Respiratory Alkalosis
Dec
Metabolic Acidosis
Inc
Metabolic Alkalosis
Respiratory Disorders- Causes of Resp Distress/Failure
Upper Airway
● Croup/Epiglottis:
○ Tx:
■ Dexamethasone
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
○
○
■ Humidified oxygen
■ Nebulizer (racemic epinephrine for stridor)
■ Intubate as needed
■ Tracheostomy as needed
Epiglottitis: Life-threatening emergency! ; acute, severe inflammation of epiglottis w/ abrupt onset &
rapid progression; caused by bacterial respiratory infx (no throat cultures!!!) can progress to fully
blocked off airway
■ Ask if child’s immunizations are up to date
■ S/S:
● Difficulty speaking & swallowing
● Sore throat
● Drool, croaking, or inspiratory stridor
● Chin thrust out
● High fever
● Restlessness, anxiety
● Neck hyperextension
● Tripod position/sitting forward
● X-ray shows epiglottal enlargement (Thumb sign)
■ Tx:
● Do NOT put anything in their mouth
● Allow pt to sit on parent’s lap to dec anxiety, don’t upset pt, allow parent to STAY w/
child
● Have tracheostomy and intubation equipment readily available
● IVF, IV antibiotics, IV corticosteroids
● 7 to 10 day course of oral antibiotics after IV therapy
■ Education: Keep pt calm and dec stimuli as much as possible; importance of Hib
(Haemophilus Influenzae type b) vaccine
● PREVENTION = IMMUNIZATIONS
Croup: From viral resp infections; inflammation of larynx, trachea, & bronchi
■ S/S:
● Abrupt and worse at night
● Mild cold a few days before
● Barky, brassy cough
● Hx of URI
● Inspiratory stridor
● Resp distress
● Low grade fever
● Tracheal narrowing on x-ray (Steeple Sign)
■ Tx For Croup:
● Allow parent to STAY w/ child
● Don’t upset child; allow position of comfort
● Cool mist oxygen therapy
● Nebulized epinephrine (Racemic epi)- for stridor
● Corticosteroids
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
●
●
● Encourage oral fluid intake
■ Education For Croup:
● Teach caregiver sx of resp distress
● Cool/moist air humidifier/vaporizer
● Fever 100-101 is common
● Stay w/ child and keep calm
● Infx prevention = Hand washing
Foreign Body: Treatments:
○ Back slap/abdominal thrusts (Heimlich)
○ Suction
○ Expert consultation (Radiology studies; endoscopy)
○ Tracheostomy as needed
Anaphylaxis: Exaggerated hypersensitivity reaction to a trigger
○ S/S:
■ Itching, Hives
■ Cough
■ Dyspnea
■ Pale/pallor
■ Stridor
■ Wheezing
■ Sweating
■ Tachycardia
■ Respiratory distress could lead to failure
○ Tx:
■ Epinephrine IM, SQ, ET
■ Nebulizer
■ Diphenhydramine (Benadryl)
■ Corticosteroids (Methylprednisolone)
■ Antihistamines
■ Fluids
■ Oxygen
■ Allow position of comfort
○ Education: Know/avoid triggers & always carry epi pen
Lower Airway
● Bronchiolitis (RSV): Obstruction of small airways (bronchioles) d/t acute URI; seasonal illness
starting in fall & ending in spring (oct to april); spread by direct CONTACT w/ secretions
○ Causes: Viral resp infx (RSV- Respiratory Syncytial Virus), Parainfluenza, Adenovirus,
Rhinovirus, Re-infection)
○ Sx of Bronchiolitis (RSV):
■ Fever low grade
■ Cough
■ Wheezing
■ Rhinorrhea
■ Retractions
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
●
■ Crackles
■ Dyspnea
■ Tachypnea
■ Snot/stuffy; copious nasal secretions
○ Tx of Bronchiolitis (RSV):
■ Naso/nasopharyngeal suction secretions PRN, esp before feedings
■ Oxygen (heating, humidified, high-flow nasal cannula [ex: optiflow, vapotherm],
hydration) [*primary tx for viral bronchiolitis is humidified o2]
■ Admin 40% high-flow oxygen via nasal cannula at 8 LPM
■ Allow position of comfort
■ Small frequent feedings & oral fluids
■ IVF if unable to take adequate PO
■ May trial bronchodilators
■ Teach caregivers:
● Prevention w/ GOOD hand washing
● Bulb suction technique
● Suction prior to each small frequent feeding
Asthma: Chronic inflammatory disorder of airways recurrent w/ acute exacerbations; reversible
episodes of obstructed by inc reaction of airways to stimuli; most common cause of missed school
days b/c of exacerbations by viral infx or env. triggers
○ Causes: Triggers: Viruses (most common), pollen/mold, cold air, exercise, cig smoke,
chemicals, scented products, weather change, infections, dust mites, cockroaches, pets
○ S/S of Asthma:
■ Wheezing
■ Coughing esp at night, after physical activity, lasting >1 wk
■ Anxiety
■ Chest tightness
■ Dyspnea
■ Use of accessory muscles
■ SOB
■ Answering in 1-2 word sentences
■ Resp distress
■ Talk in short sentences
■ Tripod
○ Dx of Asthma:
■ Pulmonary Function Test (PFT)
■ Peak Flow Meter (PFM) used to determine
“personal best” respiratory fxn, as a daily
measurement for asthma action plan and guide for
tx
○ Tx of Asthma:
■ Oxygen
■ Bronchodilators (short and long acting)
■ Nebulizers (albuterol and ipratropium bromide)
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
■
■
■
■
■
■
■
■
■
Corticosteroids
Anticholinergics
Mag sulfate
Epinephrine SQ
Support breathing
Heliox
Allow for position of comfort
Anticholinergics
Fluids
Education for Asthma:
■ Compliance w/ tx plan & trigger mgmt
■ Med use & delivery:
● Controller vs Rescue meds
● Rinse mouth after inhaler
● Giver bronchodilators first prior to steroid inhalers
● Asthma Action Plan- when to take meds & call/see PCP
● Peak Flow Meter use and monitor PF daily
■ For school age child w/ severe persistent exercise-induced asthma: Take 2 puffs of
albuterol inhaler prior to physical education daily & communication w/ school
regarding asthma action plan
Cystic Fibrosis: Genetic disorder that affects resp, GI, integumentary, and endocrine/reproductive
systems (does NOT affect the MSK system); Autosomal recessive
○
●
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
○
○
○
S/S of Cystic Fibrosis:
■ Respiratory:
● Wet, chronic cough
● Wheezing, dyspnea
● Clubbing; hypoxia; barrel chest; frequent bacterial infections
■ GI:
● Mucus blocks pancreatic ducts so unable to digest fats
● Meconium ileus at birth
● Bulky, fatty, foul smelling stools
● Delayed g&d
● Thick/sludge on mucosa so dehydration worsens resp and GI
■ Endocrine/Reproduction:
● Excess sweat from sweat glands
● Delayed puberty (female)
● Viscous cervical secretions so difficulty getting pregnant (female) (but if they
do, they have higher chance of passing it along)
● Sterile (males)
● May develop diabetes d/t pancreatic scarring
■ Liver: Inc LFTs and gallstones
■ Integumentary: Excess sodium loss from sweat glands
Dx: Sweat chloride test, DNA testing, PFT, stool analysis
Tx of Cystic Fibrosis:
■ Anticholinergics
■ Resp: Chest physiotherapy, bronchodilators (albuterol & ipratropium), aerosolized
pulmozyme- dec viscosity of mucous
■ Antibiotics (PO/IV/INH); oxygen
■ GI:
● Diet of high sodium, high fat, high calorie, fat soluble vitamins
● Avoid large amounts of sugar b/c CF prone to insulin resistance
● Pancreatic enzymes immediately prior to meals & snacks to help w/ fat
malabsorption
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
○ Pancrelipase w/ all meals & snacks
● Extra enzymes for high fat foods; vitamins A, D, E, and K
■ Endocrine: Diabetes mgmt as applicable
■ Integumentary: Replace lost electrolyte as applicable (risk heat exhaustion)
○ Education:
■ Compliance w/ tx plan (resp, meds, GI enzymes, diet, resp therapy)
■ Encourage physical exercise program
■ Follow-up w/ specialist care team (pulmonology, endocrinologist, resp therapist, care
coordinator, gastroenterologist)
■ Genetic counseling, Resources & support services
Lung Tissue Disease:
● Pneumonia: Primary infx or aspiration (chemical or vomitous) from bacterial or virus
○ S/S:
■ Fever (febrile or hypothermic)
■ Chest pain
■ Tachypnea
■ Hypoxia despite oxygenation
■ Inc work of breathing
■ Dec saturations despire inc in o2 delivery/ventilation mode
■ Course or crackles (junky)
○ Tx:
■ Antibiotics (bacterial) after sputum culture sent
● Priority tx for bacterial pneumonia dx is admin IV abx
■ Nebulizers
■ Support breathing
■ Antipyretics to treat fever
■ Oxygen
■ Pulmonary toileting (CPT, breathing treatments, suction, etc)
■ If wheezing, consider bronchodilator
○ Family Education:
■ S/S to watch for and when to return to the PCP or ED
■ Med admin instructions
■ Encourage hydration & rest
● Pulmonary Edema Tx: Diuretics, Inotrope, support breathing
CNS Issues:
● Trauma: Tx: Neurosurgery; Reduce intracranial pressure; Support breathing
● Neurological/Neuromuscular Disorder
○ Causes:
■ Trauma (closed head injury)
■ Neuromuscular disease (muscular dystrophy, SMA)
■ Central hypoventilation syndrome
■ Seizures
■ Hydrocephalus
○ Support breathing (manual BVM ventilation, BiPAP, CPAP)
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Treat the cause- seizure meds, etc
S/S:
■ Variable RR and effort
■ Respirations become ineffective causing inability to oxygenate/ventilate
○ Tx: Support breathing; Treat cause (neurosurgery to dec ICP, seizure meds, etc)
● Pharmacological/Chemical: Any medical either given or potentially taken
○ S/S:
■ Variable RR and effort
■ Respirations become ineffective causing inability to oxygenate/ventilate
○ Tx:
■ Support breathing
■ Reversal Agents/Antidotes:
● Naloxone (Narcan)- Opioid reversal
● Flumazenil (Romazicon)- Benzodiazepine reversal
■ Do NOT reverse anti-seizure meds
Otitis Media
● Risk Factors:
○ Hx of recent upper resp infx
■ Immature Eustachian tubes -> easily collapse = fluid buildup (neg. pressure) ->
bacteria growth
○ Immature immune system
○ Eustachian tube characteristics
○ Exposure to 2nd hand smoke (passive smoke) irritates Eustachian tube causing
inflammatory response
○ Day care attendance: Exposure to other children, close contact -> cross contamination +
immature immune system
○ Bottle feeding/bottle propping
● S/S of Otitis Media:
○ Ear pain esp when lying down
○ Tugging/pulling at an ear
○ Fussiness/irritability (loss of appetite in infants)
● Tx of Otitis Media: Defer tx 24-72 hours = may resolve spontaneously
○ If child under 6 mo. and has had symptoms over 72 hrs, start w/ abx therapy
○ Oral abx: Amoxicillin is 1st line; Augmentin is 2nd line
○ Manage pain w/ ear drops and fever w/ antipyretic
○ Myringotomy w/ tympanostomy tubes for recurrent infx
■ Chronic recurrent infections = risk for conductive hearing loss
Tonsillitis: Inflammation of tonsils; may also include adenoids
● Cause: Streptococcus
● S/S of Tonsillitis:
○ Enlarged, swollen tonsils
○ Difficulty swallowing
○ Difficulty breathing if severe
● Tx of Tonsillitis: Abx, support airway; tonsillectomy & possible adenoidectomy
○
○
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Post-op Nursing Care:
■ Observe for bleeding post-op and after discharge
● Clue = frequent swallowing or clearing of throat
■ No red or purple tinged fluids
■ No straws!!!
Bronchopulmonary Dysplasia (BPD): Breathing disorder where infant’s lungs become irritated and don’t
develop normally; can be mild, moderate, or severe
● Mostly in low-weight infants born more than 2 mo early
● Chronic lung disease that can result in resp insufficiency
● Many fully recover while others may have breathing difficulties in 1st two years of life & into
teen/adult years
● Infants + toddlers w/ BPD are at HIGHER risk of developing complications from viral resp
illnesses (RSV, flu)
○
4 questions
Key points: https://twu.instructure.com/courses/2934916/files/170956794/download?download_frd=1
Cardiac Disorders.docx
CHD.docx
Peer Tutor Notes: Cardiac Disorders (1).docx
Most important assmt finding in kids w/ cardiac disease = Perfusion
Acquired Heart Diseases: Kawasaki Syndrome, Rheumatic Fever, Endocarditis, Myocarditis, Pulmonary
Artery Hypertension (Game: https://www.classtools.net/vortex/202009-eZPDAg )
*Congenital = born w/ it while acquired means they were normal beforehand
Endocarditis: Happens to ppl who already have issues w/ heart
● Risk Factors: CHD, Artificial valves, central lines, nose/tongue piercings, tattoos, IV drug abusers
● Diagnosed by s&s of infection or flu (febrile, NV, aches, pain, SOB, cough, dec appetite)
○ Long term abx (cillins, mycins) required for bacterial endocarditis (6 wks)
○ May need valve replacement
○ Must maintain good dental health
○ Prophylaxis before surgery and dental visits (no longer done in adults but still done in kids)
● Sx:
○ Fever
○ Malaise
○ New onset murmur
● Commonly prescribed 5-6 weeks of IV abx
Myocarditis: Ineffective process invading myocardium after
systemic infx in normal child
● Main sx is failure to bounce back after viral infx
● ⅓ ⅓ ⅓ rule for these children
○ ⅓ have mild case, recover, and be fine
○ ⅓ will get sick, require extensive support but recover
○ ⅓ will get gravely ill w/ significant medical support up to and including a transplant
Cardiomyopathy
● Many causes: post myocarditis, congenital heart disease, HTN, many idiopathic (unknown cause)
● Monitor pt & treat depending on sx severity
● Treated similarly to adults
Past Comprehensive Content- Cardiac
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Kawasaki Disease: Mucocutaneous lymph node syndrome; unknown cause, rarely get it twice
● Dx: Fever > 5 days & at least 4 of the 5 following physical findings w/ no other more reasonable
explanation for observed clinical findings:
○ 1) Bilateral conjunctival injection
○ 2) Oral mucosal changes (erythema of lips or oropharynx, strawberry tongue, or drying or
fissuring of lips)
○ 3) Peripheral extremity changes (edema, erythema, or generalized or periungual
desquamation) **usually painful
○ 4) Rash
○ 5) Cervical lymphadenopathy > 1.5 cm in diameter
● Clinical Manifestations of Kawasaki:
○ Typical child under 5 yr, asian, sudden onset of high fever
○ Non-infective conjunctivitis: non-purulent, bilateral
○ Changes in lips and oral cavity
■ Reddening and fissuring of lips
■ Erythema of buccal mucosa
■ Strawberry tongue
○ Polymorphous Exanthem: Morbilliform, scarlatiniform or erythema multiforme; evanescent
in some pts
■ Begins in diapers area and spreads to torso and extremities upwards starts to bleed
○ Acute Phase changes in extremities (1-2 weeks) 1st 10 days w/ high fever
■ Erythema and edema of hands and feet
■ Swelling of proximal interphalangeal joints of hands
■ Constant pain and discomfort
■ Refusal to move hands or bear weight
○ Subacute Phase: After 10 days; swelling of hands/feet (kid will refuse to walk/feed self)
■ Desquamation
■ Starts in subungual regions; spreads to psalm, soles & diaper area
■ Gangrene of fingers and toes
■ Occurs rarely in very young infants of non-asian background
○ Convalescent Phases (several months to years- begins 6-8 wks after onset): Time span may
be more rapid w/ IVIG dosing
■ Sx start to disappear
■ Labs normalizing
■ Possible (not always) resolution of aneurysms; aneurysms may develop
■ May have persistent arthritis
○ Aneurysms 1st noted 12-28 days after onset of disease & rarely appear after 28 days of
onset
■ Echocardiogram required for all pts dx w/ kawasaki b/c can develop aneurysms
■ Aneurysms may thrombose leading to MI & death
■ Aneurysms may rupture (rarely)
■ A pancarditis is often present in the 1st 10 days of illness; pericardial effusions may
accompany this
■ Can end up needing bypass surgery/ CABG
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
■ New murmur is priority concern b/c pt at risk for coronary artery aneurysms
○ Kawasaki Nursing Care:
■ Bedrest for until afebrile for > 72 hours and pain diminished
■ Become familiar w/ IVIG administration
■ Provide oral care & analgesia
■ Educate family of importance of follow up
○ Management of Kawasaki:
■ Discharge teaching for family to understand weaning aspirin
● Anti-inflammatory argent ASA 80-100 mg/kg/day to wean after 2 weeks
but keep taking up to 8 weeks
■ IVIG given once at hospital
● If given w/i acute phase reduces fever and prevents aneurysms
● 1 to 2 gms/kg in one time dose over hours
● Infusion rate12
● NO live virus vaccines for 11 months after IVIG
● Follow up cardiac cath/echo to eval/rule out coronary artery aneurysms; 1st
ECHO done day after admit
○ Watch for aspirin toxicity and immunosuppression
○ Prothrombotic State
Rheumatic Fever/Rheumatic Heart Disease
● Cause: Auto-immune reaction to group A beta-hemolytic streptococcus (pharyngitis), untreated
strep throat
● Prevention: Throat cultures, prompt/total tx for strep throat
● Strep migrates to myocardium (valves), joints, skin, CNS several wks later
● Many pts with RF develop rheumatic heart disease
● Presenting Sx:
○ Small non-tender painless nodules under skin/on joints
○ New murmur
○ Unexpected jerking (chorea)
○ Pain in one joint that moves to another joint
○ Painful or sore joints in wrists, elbows, knees, and ankles
○ Stomach pain
○ Nosebleeds
○ Lethargy or fatigue
○ Chest pain
○ Rapid fluttering or pounding chest palpitations
○ Fever, red, raised rash on chest
● Valve Damage
○ Mitral valve may get injured or aortic valve
○ Poor valve fxn may produce CHF
○ Valve damage may resolve or be permanently damaged
● Diagnostic Testing for RF/Rheumatic Heart Disease:
○ EKG (16 lead, left AND right side)
○ ECHO
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
○
○
Cardiac catheterization w/ sedation
Labs to know
■ CBC: H/H, differential to see if infected process going on
■ C-Reactive Protein (CRP): inflammatory process
■ Erythrocyte Sedimentation Rate (ESR): inflammatory process
■ Anti-streptolysin- O antibody titer (ASO/ASLO): Positive tier means strep
CHF: Heart can’t pump enough O2 blood to meet needs of body’s other organs + Clinical syndrome where
heart is unable to pump enough blood to dispose of venous return adequately (Combo of the 2)
● CHF & shock are similar in that they both are conditions of cardiac output that’s inadequate to meet
metabolic body demands
● Causes: Cardiomyopathy, inc pulm blood flow defects, pressure/volume overload, endocarditis,
CHD, infx of myocardium/valves, anemia, high cardiac output such as septic shock, chronic lung
disease, HTN, diabetes
● Sx: Same as adult CHF; Impaired myocardial fxn
○ Tachycardia, gallop, diaphoresis, dec perfusion, cardiomegaly on CXR, fatigue, poor
feeding
○ Pulmonary congestion
○ Tachypnea, cyanosis, resp distress, pulmonary edema on CXR, orthopnea, wheezing, cough
○ Systemic venous congestion
○ Hepatomegaly, edema, wt gain, ascites, pleural effusion
● S&S in Infants w/ CHF:
○ Poor feeding of recent onset
○ Tachypnea that worsens during feeding
○ Vomiting w/ feeds
○ Poor wt gain
○ Cold sweat on forehead
○ Irritability
● S&S in Older Children w/ CHF:
○ SOB, esp. w/ activities
○ Puffy eyelids (periorbital edema- swelling around eyes)- seen first
○ Swollen feet
○ Easy fatigability
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
●
●
●
CXR will look very white b/c full of fluid & may see enlarged heart
Do ECHO, 12 lead ECG, cardiology consult
Goals of CHF Mgmt & Nursing Considerations: Same as an Adult!
○ Improve cardiac fxn
■ Medications: Digoxin, afterload reduction, IV inotropes
○ Diuresis/fluid restriction
■ Lasik; strict I&O, monitor electrolytes closely
■ Fluid and sodium restriction (usually in older children)
○ Decrease metabolic O2 demands
■ Conservation of energy (clustered care)
■ N/G feeds (PO requires energy and may be difficult w/ tachypnea)
■ Normothermia
○ Improve tissue oxygenation
■ Possibly admin O2
■ Reduce work of breathing, proper positioning
Left Sided HF
Right Sided HF
Pulmonary venous engorgement
Systemic venous engorgement
Tachypnea
Hepatomegaly
Grunting
Splenomegaly
FTT (Poor feeding for infants)
Pitting edema
Orthopnea in older child
Periorbital edema or distended neck veins (not visible in infants.. Necks are
not visible!!
Wheezing/rales
Congenital Heart Disease: Group of CV malformations from abnormal structural development of
heart/persistence of fetal vessels; unknown/multifactoral etiology (Game: https://bit.ly/3dIIkJ0)
Gestational/Natal Hx:
● Infx (maternal rubella, CMV, herpes virus, coxsackievirus B)
● Meds (amphetamines, phenytoin, trimethadione, lithium, thalidomide)
● Maternal conditions (diabetes, maternal lupus erythematous, mother has CHD, maternal age over
40), excessive smoking alcohol consumption
● Birth wt
Fhx: Hereditary disease, CHD, rheumatic fever, sudden unexpected death, DM, arteriosclerotic heart
disease, HTN, long QT syndrome, Marfan’s syndrome
Hx Taking in CHD: S&S:
● Feeding problems (Failure to Thrive)- irritability and poor eating
● Dysphagia
● Dyspnea
● Cyanosis
● Exercise intolerance: eating is exercise so don’t want wasting too much calories with PO feed
Physical Exam: Assess for: Growth failure, color, diaphoretic, tachypnea, tachycardia, hepatomegaly
Genetic Pattern in CHD: Inc chance if….
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Sibling(s) w/ heart defect, parent(s) w/ CHD, chromosomal aberration (Down’s Syndrome), another
non-cardiac congenital anomaly
Associated Defects:
● Tracheoesophageal fistulas, renal agenesis, diaphragmatic hernia
● Chromosomal Abnormalities: Down Syndrome, Turner Syndrome
CHD Mgmt:
● Refer to pediatric cardiology
● Most important concept for pts w/ CHD is to Feed & Grow
○ High cal formula or forfeited breast milk
● RN Role:
○ Was the CHD diagnosed prenatally? Had more time to absorb/understand it
○ Reducing parental anxiety: the blame game
○ Recognize that kids w/ chronic illness have an inc in sibling rivalry, hostility, & anger btwn
ill child and healthy child
○ Kids w/ CHD are more social isolated than other kids w/ chronic illness
○ Infants w/ CHD difficult to feed & slow to grow r/t patho and infant’s behavioral
contribution to feeding interaction
○ Monitor developmental milestones
○ Immunization status
○ Inc divorce rate in parents of kids w/ CHD
○ Cluttered Care!
○ Help families deal w/ common threads (fear, isolation, shock, anger [stages of death],
overwhelmed, attempts to place guilt/blame)
CHD Pressure Gradients: Lower on right side v. left side of heart
● Resistance: Lower in pulmonary circuit v. system circulation
● Presence of abnormal communication: Leads to shunting from higher pressure circuits to lower
pressure circuits (left to right)
Palliation: Series of surgeries for pt to live but CAN’T fix heart to look/fxn normally
Correction: Corrective surgery; Heart defect completely gone & heart looks/fxns normally
●
Heart Defect: Classifications
●
Inc Pulmonary Blood Flow: Left to Right Shunts (acranotic: pink) Holes in heart septums w/ or
w/o valve issues; since blood is lazy & flows from high to low pressure, all holes mean there’s more
blood on right side so more blood going to lungs than out to body demonstrated as CHF (exercise
intolerance all ages) in babies that means poor eating & failure to thrive; Knowing CHF sx =
Knowing inc pulm blood flow defects presentation
○ Sx of Inc Pulm Blood Flow:
■ Tachypnea
■ Subcostal and intercostal retractions
■ Nasal flaring
■ Crackles
■ 1kg weight gain over 2 days
○ Atrial Septal Defect: Opening btwn the atria
■ Most common complication is CHF
○ Ventricular Septal Defect: Opening btwn ventricles
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Patent Ductus Arteriosus: Failure of ductus arteriosus to close
Atrioventricular Canal Defect: Opening btwn atria, ventricles, & 1 common A-V valve
Sx Tx of:
■ CHF
■ Failure to thrive
■ Oxygenation
○ Cath lab or surgical repair (Correction): Better to put off surgery so they grow more
■ Close the holes
■ Fix valves if there’s an issue
■ Expect normal heart/vital signs post op depending on palliative/corrective
○ Post-op Problems:
■ Holes or valves might remain leaky
■ Heart block temporarily
■ If electrical conduction was cut, heart blocks or arrhythmias in that area
Dec Pulmonary Blood Flow: Right to Left Shunts (cyanotic) No flow to pulmonary arteries means
blood will go from right to left since now lazy blood will prefer to go to high pressure side since
easier than trying to get to pulm artery. When pts have dec pulmonary blood flow & NO holes in
septum, life gets scary & surgery will be needed w/i first few days of life.
○ Tetralogy of Fallot: Hole in ventricular wall (septum) + narrowed pulmonary outflow =
blue baby/hypercyanotic spells. Right ventricle hypertrophic b/c working hard from
beginning to move blood around; the hold btwn the ventricles has made it easy for aorta to
sit btwn the 2 ventricles rather than on left side where it belongs. So the 4 defects are: VSD
(hole in ventricular septum), narrowed pulm outflow tract (blood can’t get to lungs), RV
hypertrophy, and overriding aorta.
■ S&S:
● Hypercyanotic (Tet spells)- kid gets upset (trigger), cold, sick, fell ->
clamps down and blood cycle changes; Hypoxia -> acidosis -> more
vasoconstriction
○ Tx: Give O2, morphine, Beta blocker propranolol
● Cyanosis
● Dyspnea on exertion
● Clubbing
● Squatting
● Harsh systolic murmur
● CHF uncommon
■ Symptomatic Tx of:
● Tet spells
● Failure to thrive
● Oxygenation
■ Baby agitated & begins to turn blue -> perform knee to chest positioning
○ Tricuspid Atresia
Obstructive Lesions
○ Pulmonary valve stenosis
○ Atresia: Blocked
○
○
○
●
●
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Stenosis: Some gets through but not a lot
Coarctation of Aorta: Narrowing at patent ductus arteriosus
■ Dx w/ 4 extremity blood pressure
● Hands/radial will have significantly better blood supply/BP; 3+ bounding,
brisk cap refill, warm hands
● Feet/pedal will be cool, 3 or 4 sec cap refill, 1+ pedal pulses
○ Symptomatic Tx of:
■ Hypoxia
■ Failure to thrive
■ Dec perfusion
● Complex Lesions: Combo of any of the above; need surgeries quickly at beginning of life to
survive
○ Transportation of Great Arteries/Vessels
○ Truncus Arteriosus (TRU)
○ Total/Partial Anomalous Pulmonary Venous Return (TAPVS, PAPVR)
○ Hypoplastic Left Heart Syndrome (HLHS): Born w/o left ventricles
○ Symptomatic Treatment of:
■ Failure to thrive
■ Hypoxia
■ Dec perfusion
Observations to Note:
● Fluids are lazy & will always go path of least resistance
● No FLOW, No GROW! If poor perfusion to area in utero, area will be small/absent at birth
● Feed & Grow: All cardiac babies have growth issues & getting them big enough for surgeries is a
priority! Inc calories: 30 kilocalories per ounce of formula
● Ductal Dependent Lesions require a PDA or they die (until repaired/paliated)
Family Education in CHD Children Care:
● Identify primary caregivers (may or may not be the parent)
● CPR
● When to call pediatrician vs cardiologist vs 911
● Incision care/Sternal care (sternal precautions)
● HLHS parents have more education than others: Safe-at-home program
● Feeding tube insertion & care: Formula/breast milk supplements to increase calories/oz
● Med Admin: Draw up correctly, know actions & SE, know if OK to re-admin in times of emesis,
when to hold meds (diuretics w/ N/V)
○
○
Abuse https://docs.google.com/document/d/1LOWeY5h3cDlGay3eZzkoOfaxVQlJB1Gg8vTcJmrdV6Q/edit
0-3 yrs most deaths
Child's emotional response is not indicative of degree of abuse just poor coping
Unusual ownership of money/gifts, compulsive obsessive behaviors, sudden refusal to sleep in own bed
Physical abuse
● Punishment can result in death/injury even if unintentionally; bruising on legs, genitals, upper arms,
torsos, places that can be concealed
Downloaded by Katherine Mills (millskatherine37@gmail.com)
lOMoARcPSD|28697339
Bruising on torso, ears, or neck are concerning or any bruising on baby not able to pull or
walk (baby can’t hurt themself b/c can’t go anywhere)
● Burns same locations as punishment bruises
○ Immersion: From hot water
○ Pattern: Iron
● Fractures: Extremity fractures for non-mobile infants; scapula, sternum, ribs
● Head trauma: Severe retinal hemorrhage
● Conditions that may be confused with abuse are mongolian spots, vit K deficiency, stork bites
Seuxal abuse: Sudden onset of bed wetting after 6 mo dry spell
● Preschool children: Clingy or baby-talk
● School age: Poor peer relations, cruelty to animals, arson, stomachaches, headaches
● Adolescents: Pseudo-mature, hypersexual, confusion of sexual identity
Emotional abuse: Excess demands on child (expecting too much of child)
Chronic neglect -> brain development, cognitive fxn, poor social relations, no basic needs, non-appropriate
clothing for weather
As a nurse: Legally reliable to report suspicions of abuse within 48 hours and don’t try to interview
○
Most missed questions on Exam 1:
https://twu.instructure.com/courses/2934916/files/171748632?module_item_id=57060323
CHF, asthma, CF
Downloaded by Katherine Mills (millskatherine37@gmail.com)