Netter’s Obstetrics and Gynecology 3rd Edition - Asthma in pregnancy
advertisement

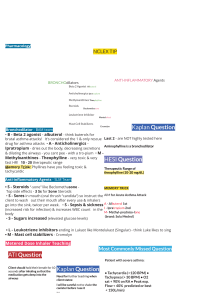
25 ASTHMA INTRODUCTION Pathologic Findings Description: Asthma (from the Greek for “panting”) is an intermittent or chronic obstructive tracheobronchial condition that is characterized by wheezing or cough. Adult-onset asthma is more common in women and poses potential problems during pregnancy. Prevalence: Seven percent of the United States population. Predominant Age: Adults aged 16–40 years (50% of patients are younger than 10 years). Genetics: Familial association with reactive airway disease, ectopic dermatitis, and allergic rhinitis. Narrowing of large and small airways because of bronchial smooth muscle spasm, edema, and inflammation of the bronchial mucosa with increased mucus production characterize acute attacks. Chronic inflammatory changes are histologically observed. Biochemical factors related to inflammation mediators include chemical, eosinophil, and neutrophil chemotactic factors, bradykinins, and others. ETIOLOGY AND PATHOGENESIS Causes: Allergic factors (airborne pollens, molds, house dust, animal dander, feather pillows; a 2004 study showed that 71% had more than one allergy and 42% had more than three allergies), smoke or pollutants, viral upper-respiratory infections, aspirin or nonsteroidal antiinflammatory agents, exercise, gastrointestinal reflux. Risk Factors: Family history and viral pneumonitis in infancy. SIGNS AND SYMPTOMS • • • • • • • Shortness of breath Wheezing and coughing (one or both) Prolonged exhalation Decreased breath sounds, hyperresonant chest Periodic (especially nocturnal) attacks Cyanosis and tachycardia Pulsus paradoxus, accessory muscle used for breathing, flattened diaphragm on chest radiograph or physical examination Symptoms are usually worse at night and in the early morning. Up to 40% of asthmatic women of childbearing age may experience a cyclical exacerbation of asthmatic symptoms during the perimenstrual period. DIAGNOSTIC APPROACH Differential Diagnosis • Recurrent pneumonia • Chronic bronchitis • Viral or fungal infection • Aspiration (foreign body) • Cystic fibrosis • Tuberculosis • Mitral valve prolapse • Congestive heart failure • Chronic obstructive pulmonary disease Associated Conditions: Reflux esophagitis, sinusitis. Workup and Evaluation Laboratory: Complete blood count, arterial blood gases (severe cases). Imaging: No imaging indicated. (Chest radiograph shows hyperinflation, atelectasis, or air leak, but it is nonspecific.) Special Tests: Sweat chloride test (childhood), nasal eosinophils, pulmonary function testing (peak expiratory flow rate), allergy testing (selected patients). Diagnostic Procedures: History, physical examination, pulmonary function testing (forced expiratory volume in 1 second, or FEV1). An excellent office screening test is to ask the patient to blow out a lit match held at arm’s length. Patients with reduced FEV1 are unable to accomplish this task. 56 MANAGEMENT AND THERAPY Nonpharmacologic General Measures: Evaluation, eliminate irritants, education, caffeine for mild symptoms. Specific Measures: Mild—intermittent β-agonists via inhaler or cromolyn sodium four times daily plus low-dose inhaled steroids (beclomethasone dipropionate 400 mg/day) may add slow-release xanthines, leukotriene modifiers (montelukast, zafirlukast, pranlukast, and zileuton). Methylxanthines (theophylline and aminophylline), if sufficient control cannot be achieved with inhaled glucocorticoids and long-acting β-agonists alone. Severe—cromolyn sodium plus high-dose inhaled steroids plus theophylline (therapeutic level 10–20 mg/mL), inhaled β-agonist to reverse airflow obstruction. During asthma attacks, patients should avoid fluid loading, intermittent positive pressure breathing, or airway mist or humidification; these worsen symptoms. Diet: No specific dietary changes indicated. Avoid known allergens (if any). Activity: No restriction or restriction based on pulmonary function, except for those with exercise-induced asthma (eg, cold weather, excessive activity). Patient Education: Understanding of disease and use of inhalers, education about triggering factors and allergens. Drug(s) of Choice • Cromoglycate and nedocromil • Steroids (beclomethasone, prednisone) • β-Agonists (albuterol, bitolterol, salmeterol, terbutaline) • Methylxanthines (theophylline) • Anticholinergics (atropine, ipratropium bromide) • Leukotriene antagonists Contraindications: Sedatives, mucolytics. Precautions: β-Agonists should only be intermittently used. Interactions: Erythromycin and ciprofloxacin slow theophylline clearance and can increase levels by 15%–20%. Alternative Drugs Histamine H1-antagonists, methotrexate FOLLOW-UP Patient Monitoring: Normal health maintenance. Prevention/Avoidance: Avoid known allergens, aspirin, nonsteroidal antiinflammatory and β-adrenergic blocking drugs. Have a prearranged action plan for acute attacks. Obtain annual influenza immunization. Avoid food additives known to precipitate attacks (sulfites and tartrazine). Possible Complications: Respiratory failure, atelectasis, pneumothorax, death. Mortality increases with more than three emergency visits or more than two hospital admissions per year, nocturnal symptoms, history of intensive care unit admission or