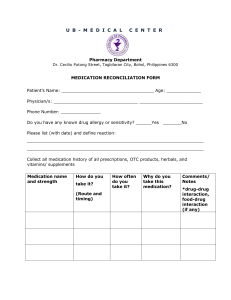
Patient Name: Jane Doe Patient Number: *outpatient facility, was not assigned* Date of birth: Admission Date: *outpatient facility* Date of Evaluation: 03/01/2023 Type of report: Comprehensive exam Attending provider: Dr. Allen Psychiatric Evaluation Identifying Information: Jane Doe is a 65-year-old African American female referred by her primary care physician, presents with bipolar manic symptoms (racing thoughts, grandiosity, and risk-taking behaviors). She lives in Hahira, Georgia, with her husband (whom she has been married to for 20 years) and ten-year-old son. She does not work, drives her appointments, and can care for herself. Positive history of inpatient psychiatric hospitalizations. Estimated Level of Intelligence: She is of average level of intelligence based on her vocabulary. Chief Complaint: “I came here because the doctor told me I talk too much and that I am busy in everyone’s business. My bitch niece said I busted in her house and been driving around town and I got a speeding ticket for nothing”. History of present Illness: Jane doe has experienced a distinct period of abnormally and persistently elevated, expansive, irritable mood and abnormally and persistent increased activity and energy that has lasted more than one week and presents nearly every day. During this period she has shown the following symptoms: inflated self esteem/grandiosity, decreased need for sleep, more talkative than usual with pressure to keep talking, flight of ideas/racing thoughts, and distractibility. The mood disturbance is sufficiently severe to cause marked impairment in social functioning yo necessitate hospitalization to prevent harm to self or others. This episode is not attributable to the physiological effects of a substance. She denies any auditory or visual hallucinations. She denies suicidal or homicidal ideations, intentions, or plans. Past Psychiatric History: She states she did partake in self harm to her wrists when she was 16 years old. She has been hospitalized 4-5 times in her life, states “those motherfuckers kept me for 10 whole days”. Her most recent hospitalization was 5 years ago. States Dr. Allen called the sheriff to have her admitted to the psychiatric hospitalization. Was once prescribed lithium and states that lithium gave her “shakes and tremors”. Also used to take Depakote but did not enjoy it because it made her gain 50 pounds. Psychiatric Review of Systems: - Mood: increased irritability, decreased need for sleep, spending sprees, increased energy and activity, flight of ideas. - Anxiety: denies - Thoughts: denies auditory and visual hallucination, grandiose delusions, flight of ideas, loose associations Family History: Mother has Bipolar disorder. Unknown of any others. Medical History: Anemia. Had a c-section with birth of her son. Current Medications: None Psychotropic Medication Black Box Warning: I have discussed the above-mentioned Medication regimen with the patient at length to include the diagnosis, target symptoms being treated, the benefits and intended outcome of treatment, the risks, side effects of each medication, known interactions with other medications and or foods, the alternative to the proposed medication treatment and the possible results of not taking the recommended medication. I have informed the patient that the medications dosages may need to be adjusted over time through the tapering dosage to prevent any adverse effects. I made the patient aware of the right to actively participated in treatment by a thorough discussion or medication concerns or questions with the prescribing provider. The patient is aware of the right to with draw voluntary consent of medication at any time unless medication in the treatment plan are required in a Court Order. Medication education was conducted for each medication ordered. The patient voiced understanding of the information presented and is in agreement with the planned medication regimen. Lab Test Reviewed: None Allergies: Lithium, Depakote Social History: Attends pentecostal church. She was raised by her grandparents, ran away from home when she was 12 years old. Her mom’s boyfriend raped her repeatedly starting at the age of 5, causing her to no longer speak or have a relationship with her mother. She states that she feels as if her mother knew she was being raped and chose to not do anything about it. She does not have a relationship with her father. She has one sibling, a sister. She only has the one marriage that she is currently in, she has a very health relationship. States her husband takes very good care of her. Developmental History: Does not recall any issues with mother’s pregnancy. Graduated highschool. Has a positive history of sexual abuse. Patient has no occupational history nor military history. Violence History: History of violence to self. Cut self when she was 16 years old. Substance Abuse History: None Legal History: Denies Trauma History: Raped by mother’s boyfriend when she was 6 years old. Review of Systems: Constitutional: No complaints ENT: No complaints Pulmonary: No complaints Cardiovascular: No complaints Gastrointestinal: No complaints Neurological: No complaints Musculoskeletal: No complaints Renal and urological: No complains Endocrine: No complaints Hematological: Anemia Skin: No complaints All other systems reviewed and are negative. Vital Signs: (Did not assess in evaluation, would have this done normally) Work History: She does not work. Mental Status Exam (With Diagnostic Impression) She is casually dressed and ambulates with normal gait and station. Speech is clear and relevant. She is oriented as evidenced by knows today’s date, time, place and current situation and able to give me that information appropriately. Her thought processes are unclear, unorganized, and racing. Her thought content was negative for suicidal homicidal ideations or any symptoms of psychosis, paranoia, delusions or persecutory thoughts. She does have flight of ideas, no thought blocking, no derailment or psychotic content. She denied auditory, visual, tactile, olfactory or gustatory hallucinations. Memory was intact for recent and remote issues as evidenced by recalling. She was not attentive with distractibility noted and interacted inappropriately during this conversation. She has poor judgment and is in denial as she believes that does not need to meet with a mental health care provider. Impulse control was inadequate based on her inability to stay on topic and not bounce from topic to topic or interrupt. No psychomotor agitation or retardation noted during the interview. ADLS: She reports he is independent of all ADLs Assets/Strength: General fund of knowledge, capable of independent living, great physical health, she lives at home with husband and son. Estimated Length of Stay: 5 days Psychiatric: Bipolar Disorder Type I, PTSD, Acute stress disorder Medical: Anemia Stressors: Her child, her husband, her doctor, “talking to you”. Substance abuse: None Mental illness: Positive history Descriptions of Attitudes and Behaviors Required to Change: She can benefit from outpatient treatment, meeting with health care provider every two weeks. Informed her it would be best to stay compliant with her medication to avoid possible hospitalization. She could also benefit from individual psychotherapy to process her childhood trauma and rape. Case Formulation: Plans and Recommendations for Treatment: Informed Jane Doe of the risks of not staying compliant with her medication and attending appointments. Prescribed Seroquel 50mg PO QHS with a follow up appointment in two weeks. Informed her that she is presenting with Bipolar Type l symptoms and went over why she meets the criteria. She does not need to be admitted to inpatient facility at this moment. Will adjust medications as needed based on clinical responses. Collateral information will be obtained as necessary. Laboratory test results will focus on education and developing coping skills to deal with stressors.Greater than 50% of this time was spent in counseling and coordination of care with this patient. Short Term Goals: Stay compliant with medication(s), stay compliant with follow up appointments, identify that she is having mental health issues. Long Term Goals: Stay out of inpatient care, decrease manic episodes, recognize and cope with triggers and stressors. Erik Erikson with Rational: Based on patient’s age and situation Jane doe is in the Ego integrity VS. Despair stage of life. “This stage takes place after age 65 and involves reflecting on one's life and either moving into feeling satisfied and happy with one's life or feeling a deep sense of regret. Success at this stage leads to feelings of wisdom, while failure results in regret, bitterness, and despair” (Mcleod, 2023). Signature of Practitioner References American Psychiatric Association. (2017). Diagnostic and statistical manual of mental disorders: Dsm-5. Mcleod, S. (2023, March 29). Erik Erikson's 8 stages of Psychosocial Development. Simply Psychology. Retrieved April 15, 2023, from https://www.simplypsychology.org/ErikErikson.html Wheeler, K. (2022). Psychotherapy for the Advanced Practice Psychiatric Nurse: A how-to guide for evidence-based practice. Springer Publishing Company.