Multiple drug allergy syndrome
advertisement

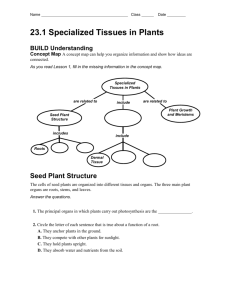
Our Dermatology Online Case Report A multiple drug allergy syndrome, multiple drug intolerance syndrome and/or allergic drug reaction with multiple immune reactants Ana Maria Abreu Velez1, Vickie M. Brown2, Michael S. Howard1 Georgia Dermatopathology Associates, Atlanta, Georgia, USA, 2 Vickie M. Brown Dermatology, Milledgeville, Georgia, USA 1 Corresponding author: Ana Maria Abreu Velez, M.D., Ph.D., E-mail: abreuvelez@yahoo.com. ABSTRACT Background: Adverse drug reactions (ADR), multiple drug allergy syndrome (MDAS) and multiple drug intolerance syndrome (MDIS), are very common in the clinical practice worldwide due to an aging population. Case report: Here we describe a 61 year old Caucasian female, who presented complaining of large, tense bullae on her right anterior arm; the bullae had been present for one week, with pruritus. The patient was taking multiple medications. The patient presented with multiple large, tense blisters and scattered, smaller blisters on her legs and axillae. Materials and Methods: Biopsies for hematoxylin and eosin (H&E) examination, direct immunofluorescence (DIF) and immunohistochemistry (IHC) analysis were performed. The H&E staining demonstrated diffuse, moderate epidermal spongiosis, with a subepidermal blister. Lymphocytes and eosinophils were present within the blister lumen and around superficial dermal blood vessels, hair follicles and sweat glands. Notably, blood vessels and lymphatics had altered shapes, many being narrowed, twisted and or dilated. DIF showed significant deposits of fibrinogen, Complement/C3c and IgA around the dermal vessels; some reactivity was also present at the basement membrane zone of the skin, as well as around dermal skin appendices. Of great interest was the reactivity seen with anti-human fibrinogen against some dermal cell junctions. IHC staining showed the presence of mainly CD4 and BCL-2 positive cells around skin appendices, with a few CD8 positive cells also present. Cyclooxygenase-2 was also very positive around the dermal blood vessels, as well as within cells of the dermal inflammatory infiltrate. The dermal lymphatics and dermal blood vessels appeared dilated, demonstrated by staining for D2-40/podoplanin and von Willembrand factor. Conclusion: Adverse drug reactions and multiple drug allergy syndrome have several overlapping features; the spectrum of immunopathologic and histopathologic features are not fully established. Our case contributes to our knowledge of some of these features. In the authors’ experience, we have noticed that the hallmark of these reactions is the prevalence of strong deposits of fibrinogen in several vessels and dermal skin appendices. In addition, we have noted positivity on some types of dermal cell junctions. MDAS, MDIS and ADRs represent examples of how to categorize adverse, simultaneous reactions to multiple classes of chemically unrelated drugs. Key words: Multiple drug allergy syndrome, multiple drug intolerance syndrome, adverse drug reactions, fibrinogen, vessels, intraepidermal blisters Abbreviations: Multiple drug allergy syndrome (MDAS), multiple drug intolerance syndrome (MDIS), adverse drug reactions (ADRs), direct immunofluorescence (DIF), immunohistochemistry (IHC), basement membrane zone (BMZ), Ulex europaeus agglutinin 1 (UEA), hematoxylin and eosin (H&E), 4’,6-diamidino2-phenylindole (DAPI), B-cell lymphoma 2 gene (BCL-2), cyclooxygenase-2 (COX-2). INTRODUCTION Multiple drug allergy syndrome (MDAS) is a clinical diagnosis made in patients with adverse reactions to two or more chemically unrelated drugs, with an underlying immune-mediated mechanism causing the reaction [1]. The term multiple drug intolerance syndrome (MDIS) has been used to describe patients who express adverse How to cite this article: Abreu Velez AM, Brown VM, Howard MS. A multiple drug allergy syndrome, multiple drug intolerance syndrome and/or allergic drug reaction with multiple immune reactants. Our Dermatol Online. 2016;7(1):40-44. Submission: 02.06.2015; Acceptance: 10.08.2015 DOI:10.7241/ourd.20161.9 © Our Dermatol Online 1.2016 40 www.odermatol.com drug reactions to three or more drugs, without a known immunological mechanism [2,3]. Thus, it is difficult in some cases to know if these nosologic entities refer to the same phenomenon. Even more confusing is to consider how single drug adverse drug reactions (ADRs) relate to a defined MDAS or MDIS case. ADRs usually affect the skin and/or mucosae (toxicoderma) [4-12], and are challenging to dermatologists, toxicologists, emergency physicians, allergists and immunologists. A better understanding of the etiopathogenic mechanisms of drug reactions is needed, and especially when these reactions are concomitant with the presence of other sequelae such as viral infections. Such non-drug reaction forces could make selected immunologic processes more complex than previously considered [5-9]. It is also believed that allergic drug reactions may have a genetic predisposition, and that epidemiologic factors can also play a role. We describe a case that exemplifies the complexity of adverse drug reactions. CASE REPORT An obese, diabetic 61 year old female presented to the dermatologist with flaccid bullae and plaques, on erythematous bases. The patient was taking Doxycycline hyclate 100 mgs caps one at day orally; Micardis HCt; oral Metformin® 850 Mgs tablets; an oral multivitamin; Symlin® SubQ, Lantus® SubQ; Novolag® SubQ. The patient described no personal or family drug allergy history. Biopsies for hematoxylin and eosin (H&E) examination, direct immunofluorescence (DIF) and immunohistochemistry (IHC) analysis were performed. After receiving the biopsy results, the patient was prescribed with econazole 1% topical cream once or twice a day, and hydrocortisone topical 2.5% lotion; the dermatologist also began working to change and/or decrease her medications in consultation with her other physicians. MATERIALS AND METHODS Skin biopsies were taken for histology (H&E) studies, for immunohistochemistry (IHC) and for direct immunofluorescence studies (DIF); our techniques were performed as previously described [7-12]. The skin was then incubated with primary and/or secondary antibodies. We utilized FITC conjugated rabbit antisera to human IgG, IgA, IgM, IgD, IgE, Complement/C1q, Complement/C3, Complement/ C4, Kappa light chains, Lambda light chains, albumin and fibrinogen. All of our antibodies were obtained from Dako(Carpinteria, California, USA) with the following details and exceptions. Our anti-human IgA antiserum (alpha chain) and anti-human IgM antiserum (mu chain) were obtained from Dako. Our anti-human-IgE antiserum (epsilon chain) was obtained from Vector Laboratories (Burlingame, California, USA). Our anti-human IgD antibodies were obtained from Southern Biotechnology (Birmingham, Alabama, USA), and utilized at dilutions of 1:20 to 1:40. The slides were counterstained with 4’,6-diamidino2-phenylindole(DAPI; Pierce, Rockford, Illinois, USA). We also used Texas Red conjugated Ulex europaeus agglutinin 1 (UEA) (from Vector Burlingame, CA, USA) as a vascular marker. The samples were consistently run with positive and negative controls. We classified our findings as negative (-), weakly positive (+), positive (+++) and strongly positive (++++). IHC double staining Our double stained IHC was performed using a double staining system; we utilized the Leica Bond Max platform autostainer with bond polymer refined Red detection DS9390, alkaline phosphatase linker polymer and fast red chromogen (red staining) as previously described [5-9]. We also used a bond polymer refined detection DS9800, horseradish peroxidase linked polymer and DAB chromogen (brown staining). The following antibodies were utilized from Dako: Mouse monoclonal anti-human CD4; CD8; CD15; CD68; B-cell lymphoma 2 gene (BCL-2) oncoprotein, clone 124; cyclooxygenase-2 (COX-2), clone CX-294; polyclonal rabbit anti-human vonWillembrand factor, and D2-40/podoplanin. The following antibodies were used from Novocastra (Chicago, Illinois, USA): anti-human CD4 clone 4B12; anti-human C8 Clone C8/144B, and von Willembrand factor. We counterstained the slides with hematoxylin. Positive and negative controls were consistently performed. RESULTS Direct immunofluorescence (DIF) Microscopic description For DIF, the skin was imbedded in optimal cutting temperature (OCT) compound for frozen-sectioning. A: Examination of the H&E tissue sections demonstrated diffuse, moderate epidermal spongiosis present. © Our Dermatol Online 1.2016 41 www.odermatol.com A subepidermal blister was noted, with small numbers of lymphocytes and eosinophils noted within the blister lumen. Significant superficial papillary dermal edema was noted. The dermis also displayed a mild, superficial, perivascular infiltrate of lymphocytes and histiocytes; eosinophils and neutrophils are rare. No frank vasculitis was present; however, some fibrinoid alterations were seen in dermal blood vessel walls (Fig. 1). a c b Direct immunofluorescence (DIF) Our DIF demonstrated the following results: IgG (+, focal dermal perivascular); IgA (++, focal dermal perivascular and faint linear basement membrane zone staining) (Fig. 1); IgM (+, focal dermal perivascular and focal epidermal); IgD (+, focal dermal perivascular); IgE (-); Complement/C1q (+, focal dermal perivascular); Complement/C3 (++, focal dermal perivascular, and focal epidermal); Complement/C4 (-); Kappa light chains (+, focal dermal perivascular); Lambda light chains (+, focal dermal perivascular and focal epidermal); albumin (+, focal punctate dot epidermal stratum corneum) and fibrinogen (++++, focal dermal perivascular, perieccrine and +, faint linear BMZ). Of interest was the positivity of some type of dermal cells junctions seen with fibrinogen (++) (see Fig. 1). Immunohistochemistry (IHC) d g e f h i Figure 1: (a) H&E stain shows a subepidermal blister (black arrow), with dermal edema and dilation of dermal vessels. (b) DIF using FITC conjugated anti-human fibrinogen, staining positive around the upper dermal vessels (green staining; white arrow). The nuclei of endothelial cells were counterstained with DAPI (light blue staining), and the vessels were stained with Ulex europaeus (orange staining). (c) An H&E stain, featuring the inflammatory infiltrate around the upper and intermediate dermal vessels (black arrow; 200X). (d) IHC staining, showing positivity of the lymphatic marker D2-40/podoplanin on lymphatic vessels around a hair follicle (brown staining; black arrow), and also neo-formation of lymphatics in the adjacent dermis (brown staining; red arrow). (e) DIF using FITC conjugated anti-human IgA, and showing positive staining against the upper and intermediate vessels (green/white staining; red arrows). The white arrow highlights the linear BMZ staining. overexpressed under the blister. (f) IHC, showing von Willembrand factor expressed and grouped under the blister (brown staining; black arrow). (g) Double color IHC, showing positive staining for with BCL-2 in brown and COX-2 in red in the inflammatory infiltrate around dermal blood vessels (black arrows). (h) zDIF, using FITC conjugated anti-human fibrinogen and showing positive staining around upper dermal blood vessels (green staining; white arrow). The vessel endothelial cells were stained with Texas red conjugated Ulex europaeus to confirm colocalization (pink/red staining). In addition, the nuclei of endothelial cells and keratinocytes were counterstained with DAPI (light blue). (i) Double color IHC, showing positive staining with BCL-2 in brown and COX-2 in red around blood vessels supplying a dermal eccrine sweat gland duct (red arrows). © Our Dermatol Online 1.2016 D2-40 seemed to be overexpressed on lymphatic vessels in areas such as under the blister, and around hair follicles and sweat glands. Von Willembrand factor staining showed that the blood vessels in the upper dermis were somehow compartmentalized under the blister (Fig. 1). CD15 was negative, as well as CD68. CD8 was positive only in small amounts around some upper dermal vessels. In contrast, CD4 was positive around several upper dermal blood vessels and around eccrine sweat gland ducts. BCL-2 followed the same pattern of positivity as CD4. COX-2 was very positive around the dermal blood vessels, as well as in other areas of the inflammatory infiltrate. DISCUSSION From the immunologic point of view, we have seen allergic skin reactions becoming more common in an aging population. These reactions involve interactions between multiple medications, and also reactions to soaps, detergents, hair dyes, shampoos, toothpastes and food preseratives [5-9]. Multiple simultaneous medications can alter how the body metabolizes the drugs, and also can produce alterations in the immune system. The ADR/MDAS/MDIS classifications are potentially more complex than the classic Gell and Coombs classification [13]. The Gell-Coombs classification divides drug hypersensitivity and other immune reactions into four categories, known as type I-IV reactions. In cases like ours, we see an immune response that features several units of the Gell-Coombs 42 www.odermatol.com classification, manifested by our COX-2, B and T lymphocytic and fibrinogen findings. Our laboratory has extensive experience with skin biopsies from patients with multiple drug reactions. In many of our ADR/MDAS/MDIS cases, we note that a histologic hallmark is the presence of fibrinoid material in the superficial and deep dermal blood vessels [9-12]. The classic immune response is demonstrated by a significant anti-human-fibrinogen antibody component. In the current case, we noted that the dermal vessels demonstrated changes in their sizes and shapes; these changes could trigger deposits from the clotting cascade. We also demonstrated that both lymphatics and blood vessels were affected by these changes. We speculate that these vessels could become immunologically active by the drug reaction damage, and molecules such as inducible COX-2 could become active in these sites [14]. It also has been reported that many drug eruptions are due to T cell-mediated hypersensitivity reactions; these reactions can involve activation of multiple pro-inflammatory mechanisms, which would explain the varied manifestations. However, other allergic drug reaction immune components have also been described [15,16]. In this context, our CD68 staining was largely negative, suggesting that significant activation of the classic antigen presenting cell pathway did not occur. Moreover, some immunologic aspects of drug reactions challenge our classical understanding of antigen processing and presentation. New immunologic hypotheses have been proposed in their study, including whether complement and/or immunoglobulins can formally alter molecules. The altered molecules could then, in theory, act as new haptens [15,16]. In our case, we also found that some of the cells staining with CD4 and CD8 were also positive with BCL-2; BCL-2 is considered an important anti-apoptotic protein [17]. In addition, recent discoveries have also noted that BCL2 molecules are indispensable for activation and maturation of T lymphocytes following antigen presentation [17]. One group of authors identified patient factors that could increase the risk of MDIS, in a total of 25,695 patients with documented drug intolerance. Their findings demonstrated that MDIS was associated with female gender, multiple comorbidities, and previous hospital admissions. A documented allergy to penicillin did not increase the likelihood of MDIS [2]. The cases seen in our laboratory also had shown agreement with these findings, especially relative to comorbidities and advanced patient age. © Our Dermatol Online 1.2016 In our experience, when a multiple drug allergy syndrome and/or allergic drug reaction is being evaluated the DIF usually demonstrates significant reactivity with fibrinogen and complement. We have noted significantly less reactivity with IgG and IgA, contrary to classic autoimmune blistering diseases that often demonstrate significant deposits of these immunoglobulins, Complement/C3 and fibrinogen at the basement membrane zone. Additionally, most linear IgA deposits at the BMZ seen by DIF in adults present in allergic drug reactions [17]. CONCLUSIONS The approach and assessment of patients with possible ADRs/MDAS/MDIS involves taking a comprehensive drug allergy history, ruling out viral or other concomitant infections [18], and immediately contacting other physicians that are treating the patient to work together to decrease the dosage of and/or discontinue some medications. ACKNOWLEDGMENTS We would like to thank Jonathan S. Jones, HT (ASCP) for excellent technical work at Georgia Dermatopathology Associates. Consent The examination of the patient was conducted according to the Declaration of Helsinki principles. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. Blumenthal KG, Saff RR, Banerji A. Evaluation and management of a patient with multiple drug allergies. Allergy Asthma Proc. 2014;35:197-203. Omer HM, Hodson J, Thomas SK, Coleman JJ. Multiple drug intolerance syndrome: a large-scale retrospective study. Drug Saf. 2014;37:1037-45. Macy E, Ho NJ. Multiple drug intolerance syndrome: prevalence, clinical characteristics, and management. Ann Allergy Asthma Immunol. 2012;108:88-93. de la Torre C, Suh Oh HJ. Advances in the diagnosis of drug eruptions. Actas Dermosifiliogr. 2013;104:782-88. Calbo S. Severe drug eruptions revisited. Immunol Res. 2012;53:162-7. Sukasem C, Puangpetch A, Medhasi S, Tassaneeyakul W. Pharmacogenomics of drug-induced hypersensitivity reactions: challenges, opportunities and clinical implementation. Asian Pac J Allergy Immunol. 2014;32:111-23. Abreu Velez AM, Jackson BL, Howard MS A. Deposition of immunoreactants in a cutaneous allergic drug reaction. North Am J Med Sci. 2009;1:180-3. Abreu Velez AM, Klein AD, Howard MS. Bullous allergic drug 43 www.odermatol.com 9. 10. 11. 12. 13. 14. eruption with presence of myeloperoxidase and reorganization of the dermal vessels observed by using CD34 and collagen IV antibodies. North Am J Med Sci. 2011;3:82-4. Abreu Velez AM, Jackson BL, Howard MS. Salt and pepper staining patterns for LAT, ZAP-70 and MUM-1 in a vasculitis bullous allergic drug eruption. Our Dermatol Online. 2011;2:211-5. Abreu Velez AM. Klein AD, Howard MS. An allergic bullous drug reaction triggered by levofloxacin and trimethoprim/ sulfamethoxazole mimicking an autoimmune blistering disease. Our Dermatol Online. 2012; 3:341-3. Abreu Velez AM, Loebl AM. Howard MS. Spongiotic dermatitis with a mixed inflammatory infiltrate of lymphocytes, antigen presenting cells, immunoglobulins and complement. Our Dermatol Online. 2011;2:52-7. Abreu Velez AM, Klein AD, Howard MS. LAT, EGFR -pY197, PCNL2, CDX2, HLA-DPDQDR, bromodeoxyuridine, JAM-A, and ezrin immunoreactants in a rubbed spongiotic dermatitis. Our Dermatol Online. 2011;2:211-5. Gell PGH, Coombs RRA, eds. Clinical Aspects of Immunology. 1st ed. Oxford, England: Blackwell; 1963. Dubois RN, Abramson SB, Crofford L, Gupta RA, Simon LS, Van © Our Dermatol Online 1.2016 15. 16. 17. 18. De Putte LB, et al. Cyclooxygenase in biology and disease. FASEB J. 1998;12:1063-73. Asero R. Detection of patients with multiple drug allergy syndrome by elective tolerance tests. Ann Allergy Asthma Immunol. 1998;80:185-8. Farsaci B, Sabzevari H, Higgins JP, Di Bari MG, Takai S, Schlom J, et al. Effect of a small molecule BCL-2 inhibitor on immune function and use with a recombinant vaccine. Int J Cancer 2010;127,1603-3. Abreu Velez AM, Vasquez-Hincapie DA, Howard MS. Autoimmune basement membrane and subepidermal blistering diseases. Our Dermatol Online. 2013;4(Suppl.3):647-62. Demoly P, Guglielmi P, Guglielmi L. Drug allergy and hypersensitivity. Risk factors. Bull Acad Natl Med. 2006;190:1733-42. Copyright by Ana Maria Abreu Velez, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Source of Support: Nil, Conflict of Interest: None declared. 44