Miami Dade College Medical Campus School of Health Sciences
advertisement

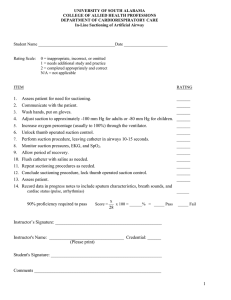
Miami Dade College Medical Campus School of Health Sciences Respiratory Care Program RET 2833 Respiratory Care Clinic 2 (Revised: May 2015) 1 2 MIAMI DADE COLLEGE MEDICAL CAMPUS SCHOOL OF HEALTH SCIENCES RESPIRATORY CARE PROGRAM RET 2833 RESPIRATORY CARE CLINIC 2 COURSE OUTLINE COURSE OVERVIEW: RET 2833 is designed to allow the student to develop psychomotor skills related to Respiratory Care. During the course, the student is provided with the opportunity to apply and discuss the theory and techniques as learned in pre-requisite and co-requisite courses. The student is also responsible for all objectives in pre-requisite and co-requisite courses. Clinic Days: _____________________ Clinic Location: ________________________ Clinic Location: ______________________ Instructor: ______________________ Office #: ______________________________ Phone #: ______________________ E-mail: _____________________________ Office Hours: __________________________________________________________ EVALUATIONS: 1st Clinic Evaluation 35% 2nd Clinic Evaluation 45% Written Exams 20% 3 RET 2833 TABLE OF CONTENTS MODULE 1.0 PATIENT DATA EVALUATION MODULE 2.0 PHYSICAL ASSESSMENT MODULE 3.0 PERFORM PROCEDURES TO COLLECT CLINICAL INFORMATION MODULE 4.0 AIRWAY MANAGEMENT MODULE 5.0 AEROSOL DRUG THERAPY MODULE 6.0 LUNG EXPANSION THERAPY MODULE 7.0 BRONCHIAL HYGIENE THERAPY MODULE 8.0 PATHOPHYSIOLOGY SKILLS LAB – TASKS COMPLETION RECORD TASKS CLINIC - TASKS COMPLETION RECORD 4 MODULE 1.0 - PATIENT DATA EVALUATION General Objective: Upon completion of the module, the student will demonstrate an ability to review data in the patient record as integral part of the overall patient assessment. Specific Objectives: 1.0 Collect, evaluate and discuss pertinent clinical information derived from the patient’s medical record: 1.1 Patient history e.g., Present illness Progress notes Admission notes Diagnoses Respiratory care orders DNR status Medication history Patient education (previous) 1.2 Physical examination relative to the cardiopulmonary system e.g., vital signs, physical findings 1.3 Laboratory data e.g., CBC Culture and sensitivities Electrolytes Sputum Gram stain Coagulation studies 1.4 Pulmonary function results 1.5 Blood gas results 1.6 Imaging studies e.g., Radiograph, CT, MRI 1.7 Monitoring data, e.g., Pulse oximetry, ECG 1.8 Sleep study results e.g., diagnosis, treatment 5 MODULE 2.0 – PHYSICAL ASSESSMENT General Objective: Upon completion of the module, the student will demonstrate the ability to perform a physical assessment. Specific Objectives: 2.0 Collect, evaluate and discuss pertinent clinical information derived from a physical examination of the patient: 2.1 Interview the patient to determine: a. Level of consciousness and orientation, emotional state, and ability to cooperate b. Level of pain c. Presence of dyspnea, sputum production, and exercise tolerance d. Social history, e.g., smoking, substance abuse e. Learning needs 2.2 Assess patient’s overall cardiopulmonary status by inspection to determine: a. General appearance e.g., Venous distention Edema Accessory muscle activity Chest wall movement Diaphoresis Cyanosis Breathing pattern b. Airway assessment e.g., macroglossia, neck range of motion c. Cough, sputum amount and character d. Apgar score, gestational age, transillumination of the chest 2.3 Assess patient’s overall cardiopulmonary status by palpation a. Pulse, rhythm, force b. Asymmetrical chest movements, tactile fremitus, crepitus, tenderness, secretions in the airway, and tracheal deviation 2.4 Assess a patient’s overall cardiopulmonary status by percussion 2.5 Assess patient’s overall cardiopulmonary status by auscultation a. Breath sounds b. Heart sounds and rhythm c. Blood pressure 6 MODULE 3.0 PERFORM PROCEDURES TO COLLECT CLINICAL INFORMATION General Objective: Upon completion of the module, the student will demonstrate the ability to perform procedure to collect pertinent clinical information. Specific Objectives: 3.0 Perform procedure and interpret results for: 3.1 Pulse oximetry 3.2 Bedside spirometry e.g., FVC, FEV1 3.3 Tidal volume, minute volume, vital capacity, and peak flow 3.4 Arterial blood sampling 7 MODULE 4.0 - AIRWAY MANAGEMENT General Objective: Upon completion of the module, the student will be able to perform various procedures related to airway management for the adult and pediatric patient. Specific Objectives: 4.1 Establish the need for and safely insert an oropharyngeal airway 4.2 Establish the need for and safely insert a nasopharyngeal airway 4.3 Establish the need for and aseptically perform nasotracheal suctioning 4.4 Establish the need for and aseptically perform endotracheal suctioning 4.5 Aseptically collect a sputum sample during nasotracheal or endotracheal suctioning 4.6 Establish the need for and perform or assist with oral endotracheal intubation; inclusive of assessment and confirmation of endotracheal tube (ETT) placement, and securing the ETT 4.7 Measure and adjust ETT or tracheostomy tube (TT) cuff pressure 4.8 Establish the need for and perform ETT extubation or TT decannulation 4.9 Aseptically perform TT and stoma care 8 MODULE 5.0 – AEROSOL DRUG THERAPY General Objective: Upon completion of the module, the student will be able to perform various procedure related to the delivery of aerosolized medications to the adult and pediatric patient. Specific Objectives: 5.1 Select the best aerosol delivery system for a given patient 5.2 Procure the correct type and dosage of ordered medication via unit dose or multi-dose vial using a syringe 5.3 Safely and effectively administer medication via a metered dose inhaler (MDI); with and without a reservoir device 5.4 Safely and effectively administer medication via a dry powdered inhaler (DPI) 5.5 Safely and effectively administer medication via a small volume nebulizer (SVN) 5.6 Safely and effectively administer medication via a continuous nebulizer 5.7 Evaluate and monitor patient’s objective and subjective responses to aerosol drug therapy 5.8 Independently modify therapeutic procedures bases on the patient’s response, e.g., terminate treatment, modify techniques, etc. 5.9 Record/Communicate therapy and results using conventional terminology as required in the health care setting and/or regulatory agencies a. Specify therapy administered, date, time, frequency or therapy, medication, and ventilatory data b. Note and interpret patient’s response to therapy i. Effects of therapy, adverse reactions, patient’s subjective and objective response to therapy ii. Ausculatory findings, cough and sputum production and characteristics iii. Vital signs iv. Pulse oximetry, heart rhythm, capnography c. Communicate information regarding patient’s clinical status to appropriate members of the heath care team 9 MODULE 6.0 LUNG EXPANSION THERAPY General Objective: Upon completion of the module, the student will perform the various procedures involved in lung expansion therapy for the adult and pediatric patient. Specific Objectives: 6.1 Establish the need for and correctly administer incentive spirometry (IS) 6.2 Establish the need for and correctly administer intermittent positive airway pressure (IPPB) using the most effective adjunct (mouth piece, mouth seal, mask, etc.) 6.3 Establish the need for and correctly administer positive airway pressure (PEP, CPAP) 6.4 Evaluate and monitor patient’s objective and subjective responses to lung expansion therapy 6.5 Independently modify therapeutic procedures bases on the patient’s response, e.g., terminate treatment, modify techniques, etc. 6.6 Record therapy and results using conventional terminology as required in t he health care setting and/or regulatory agencies a. Specify therapy administered, date, time, frequency or therapy, medication, and ventilatory data b. Note and interpret patient’s response to therapy i. Effects of therapy, adverse reactions, patient’s subjective and objective response to therapy ii. Ausculatory findings, cough and sputum production and characteristics iii. Vital signs iv. Pulse oximetry, heart rhythm, capnography c. Communicate information regarding patient’s clinical status to appropriate members of the heath care team 10 MODULE 7.0 BRONCHIAL HYGIENE THERAPY General Objective: Upon completion of the module, the student will be able to perform procedures related to bronchial hygiene for the adult and pediatric patient. Specific Objectives: 7.1 Establish the need for and correctly administer EZPAP, PEP, or Vibratory PEP (Acapella, or Flutter Valve) 7.2 Establish the need for and correctly administer postural drainage, making modifications as needed 7.3 Establish the need for and correctly administer chest percussion and vibration, making modifications as needed 7.4 Establish the need for and correctly administer High-Frequency Chest Wall Oscillation (HFCWO) 7.5 Effectively instructs, demonstrates, and assists patient in various directed cough techniques 7.6 Evaluate and monitor patient’s objective and subjective responses to bronchial hygiene 7.7 Independently modify therapeutic procedures bases on the patient’s response, e.g., terminate treatment, modify techniques, etc. 7.8 Record therapy and results using conventional terminology as required in t he health care setting and/or regulatory agencies a. Specify therapy administered, date, time, frequency or therapy, medication, and ventilatory data b. Note and interpret patient’s response to therapy i. Effects of therapy, adverse reactions, patient’s subjective and objective response to therapy ii. Ausculatory findings, cough and sputum production and characteristics iii. Vital signs iv. Pulse oximetry, heart rhythm, capnography c. Communicate information regarding patient’s clinical status to appropriate members of the heath care team 11 MODULE 8.0 PATHOPHYSIOLOGY General Objective: Upon completion of the module, the student will be able to discuss the pathophysiology related to the patient's treated during clinical rotations. Specific Objectives: 8.1 Analyze available patient data (medical record, physical exam) and determine the pathophysiologic state of the patient 8.2 Describe the main pathologic features presented by the patient and its relationship to patient's disease or condition 8.3 Determine appropriateness of prescribed therapy and goals as they relate to the pathophysiologic state of the patient and adjust therapy as per protocol, or recommend changes in respiratory care plan when indicated 12 Respiratory Care Program RET 2833 Respiratory Care Clinic 2 SKILLS LAB COMPETENCIES Student Name: __________________________ Date: ___________ MDC ID: ________________________________ 13 14 RET 2833 SKILLS LAB – TASKS COMPLETION RECORD Student Name: ________________________________________________ TASK DESCRIPTION DATE Instructor Initials INSERTION OF OROPHARYNGEAL AIRWAY DURING MANUAL RESUSCITATION OROPHARYNGEAL SUCTIONING USING A TONSIL TIP SUCTION DEVICE INSERTION OF NASOPHARYNGEAL AIRWAY / NASOTRACHEAL SUCTIONING AND SPECIMEN COLLECTION ENDOTRACHEAL TUBE/TRACHEOSTOMY TUBE SUCTIONING WITH: A. SUCTION CATHETER B. CLOSED SUCTION SYSTEM DRAWING AND MEASURING MEDICATION USING A SYRINGE INITIATION OF SMALL VOLUME NEBULIZER (SVN) ADMINISTRATION OF MEDICATION VIA A MDI / DPI CHEST PHYSIOTHERAPY - POSTURAL DRAINAGE / PERCUSSION / VIBRATION BEDSIDE SPIROMETRY INCENTIVE SPIROMETRY POSITIVE AIRWAY PRESSURE (PAP) / POSITIVE EXPIRATORY PRESSURE (PEP) THERAPY IPPB THERAPY ADMINISTRATION - BIRD SERIES DCE _______________________________________________________________ DATE ______________ Instructors will date and initial the Task Sheet Completion Record as the student successfully completes each task. The Task Sheet Completion Record will be collected by the instructor and placed in the student’s record at the end of Skills Laboratory. 15 16 INSERTION OF OROPHARYNGEAL AIRWAY DURING MANUAL RESUSCITATION STUDENT NAME: __________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Selects and gathers the necessary equipment a. Oropharyngeal airway b. Resuscitator bag-valve- mask (BVM) with oxygen tubing c. Oxygen source i. wall outlet with flow meter and nipple adaptor ii. O2 tank with appropriate regulator and nipple adaptor 2. Assembles the equipment and ensures that resuscitator is working and connected to the oxygen source with the oxygen flowing at 15 liters/minute 3. Washes hands and applies standard precautions and transmissionbased isolation procedures as appropriate 4. Assesses and verifies the patient’s need for manual resuscitation 5. Measures the patient for the appropriate size oropharyngeal airway (OPA) 6. Appropriately positions the patient’s airway using the head-tilt, chin-lift or jaw–thrust maneuver 7. Inserts the OPA using the appropriate technique 8. Applies the mask to the patient’s face, repositions the patient’s head / airway and administers a manual breath 9. Assesses the adequacy of ventilation by ensuring that the chest is expanding 10. Manually ventilates the patient at a rate of 12 – 16 breaths per minute using an I:E ratio of 1:2 11. Demonstrates how to properly hold the mask and position the patient’s head / airway with 2 hands while another students assists with manual ventilation RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ Student Signature: _________________________________________________________ Date: ____________________ 17 OROPHARYNGEAL SUCTIONING USING A TONSIL TIP SUCTION DEVICE STUDENT NAME: ______________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Collects necessary equipment: PPE, vacuum regulator, vacuum collection jar suction regulator, tonsil tip suction device, sterile H2O 2. Verifies physician's order 3. Introduces self, explains the purpose of the procedure, and confirms patient’s and/or family’s understanding 4. Decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash and dons the appropriate PPE 5. Confirms the patient’s identity and assesses the patient’s pulse, respiratory rate, and breath sounds 6. Attaches vacuum regulator to vacuum outlet, connects collection jar to vacuum regulator, connects suction connecting tube to collection jar, and connects tonsil tip suction to suction connecting tube 7. Adjusts vacuum regulator to appropriate vacuum level to facilitate the removal of oral secretions and inserts tonsil tip suction into patient's mouth, avoids gagging the patient by not advancing the tonsil tip suction too far into the back of the oropharynx 8. After completing the procedure, rinses tonsil tip with sterile H2O, turns off vacuum regulator, and stores/disposes of equipment properly 9. Repositions the patient as comfortable as possible, reassures patient, observes patient's tolerance of therapy 10. Ensures the safety and comfort of the patient before leaving patient's room 11. Removes and disposes of PPE properly and washes hands 12. Records relevant data in patient chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the heath care team RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _____________________________________________ Date: ____________________ Comments/Remedial Action Plan: _____________________________________________________________________ Student Signature: _____________________________________________________ Date: ____________________ 18 ENDOTRACHEAL TUBE (ETT) or TRACHEOSTOMY TUBE (TT) SUCTIONING WITH AND WITHOUT A CLOSED SUCTION CATHETER SYSTEM STUDENT NAME: ______________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Selects and gathers the necessary equipment: a. Resuscitator bag / mask with oxygen tubing b. Oxygen source i. wall outlet with flow meter and nipple adaptor ii. O2 tank with appropriate regulator and nipple adaptor c. Suction regulator d. Suction canister with tubing e. Suction catheter or closed catheter system f. Sterile and non-sterile gloves g. Sterile water and sterile container 2. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 3. Washes hands using the appropriate hand-hygiene procedure and initiates standard and/or transmission based precautions 4. Assesses the patient’s vital signs and breath sounds and verifies the patient’s need for suctioning 5. Assembles and checks equipment: a. Ensures that BVM is working and connected to the oxygen source with the oxygen flowing at 15 liters/minute b. Ensures that the suction system (regulator, canister, tubing) are connected and functioning properly c. Adjusts the suction regulator to the appropriate level d. Pours sterile water into sterile container 6. Places the patient in a Fowlers position and hyperoxygenates and hyperinflates the patient for at least 30 seconds using the BVM 19 ENDOTRACHEAL TUBE (ETT) or TRACHEOSTOMY TUBE (TT) SUCTIONING WITH AND WITHOUT A CLOSED SUCTION CATHETER SYSTEM PROCEDURE 7. Dons sterile gloves and connects the suction catheter to suction tubing; ensuring that the catheter does not become contaminated Satisfactory Unsatisfactory Closed sheath catheters: the catheter is already attached, simply unlock the thumb port suction valve 8. Applies suction intermittently and rotates and withdraws catheter for a maximum of 10 – 15 seconds Closed sheath catheters: Depress the thumb port suction valve to apply suction Hyperoxygenates and hyperinflates the patient using the BVM for at least 60 seconds 10. Reassesses patient’s vital signs, breath sounds, and pulse oximetry 11. Suctions normal saline solution through the catheter to clear the catheter of secretions. Repeats the suctioning and clearing processes if necessary 9. Closed sheath catheters: upon completion of the procedure, with the catheter withdrawn into its sheath, inject sterile normal saline solution through the catheter’s lavage/irrigation port while applying suction in order to clear the catheter of secretions 12. Disposes of suction catheter and sterile gloves in the appropriate biohazard container Closed sheath catheters: Retracts the catheter into its sheath and locks the thumb port suction valve to prevent accidental suctioning 13. Reassess vital signs, breath sounds, and SPO2 and ensures that the patient is comfortable 14. Removes non-sterile gloves and decontaminates hands with an alcoholbased hand rub or performs a 15 second hand wash 20 ENDOTRACHEAL TUBE (ETT) or TRACHEOSTOMY TUBE (TT) SUCTIONING WITH AND WITHOUT A CLOSED SUCTION CATHETER SYSTEM PROCEDURE Satisfactory Unsatisfactory 15. Ensures the safety and comfort of the patient before leaving patient's room 16. Records relevant data in patient chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the heath care team RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: ________________________________________________________ Date: _____________________ 21 NASOTRACHEAL SUCTIONING WITH NASOPHARYNGEAL AIRWAY (NPA) AND SPECIMEN COLLECTION STUDENT NAME: ______________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Selects and gathers the necessary equipment: a. Nasopharyngeal airway b. BVM with oxygen tubing c. Oxygen source i. wall outlet with flow meter and nipple adaptor ii. O2 tank with appropriate regulator and nipple adaptor d. Suction regulator e. Suction canister with tubing f. Suction catheter g. Sterile and non-sterile gloves h. Water-soluble lubricant i. Sterile water and sterile container j. Luken’s trap 2. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 3. Washes hands using the appropriate hand-hygiene procedure and initiates standard and/or transmission based precautions 4. Verifies patient’s identity and assesses the patient’s vital signs and breath sounds and verifies the patient’s need for nasotracheal suctioning 5. Assembles and checks equipment: a. Ensures that BVM is working and connected to the oxygen source with the oxygen flowing at 15 liters/minute b. Ensures that the suction system (regulator, canister, tubing) is connected and functioning properly c. Adjusts the suction regulator to the appropriate level d. Places the Lukens trap inline with suction tubing e. Pours sterile water into sterile container 6. Places the patient in a Fowlers position and removes any oxygen adjuncts that might be in use 7. Measures the patient for the appropriate size NPA and inserts it using the appropriate technique 8. With the assistance of a student or instructor, hyperoxygenates and hyperinflates the patient for at least 30 seconds using the BVM 22 NASOTRACHEAL SUCTIONING WITH NASOPHARYNGEAL AIRWAY (NPA) AND SPECIMEN COLLECTION PROCEDURE Satisfactory Unsatisfactory 10. Lubricates the catheter and inserts it through the NPA, into the oropharynx and into the patients trachea 11. Applies suction and rotates and withdraws catheter for a maximum of 10 – 15 seconds 12. Assistant hyperoxygenates and hyperinflates the patient using the resuscitator bag/mask for at least 60 seconds 13. Reassesses patient’s vital signs, breath sounds, and pulse oximetry readings by viewing the above-bed monitors, being vigilant of any untoward reactions 14. Suctions normal saline solution through the catheter to clear the catheter of secretions. Repeats the suctioning and clearing processes if necessary 15. Disposes of suction catheter and sterile gloves in the appropriate biohazard container 19. Removes non-sterile gloves and decontaminates hands with an alcoholbased hand rub or performs a 15 second hand wash 20. Properly labels sputum specimen and places it in a biohazard bag for transport to laboratory 21. Records relevant data in patient chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the heath care team 9. Dons sterile gloves and connects the suction catheter to suction tubing; ensuring that the catheter does not become contaminated 16. Removes the Lukens trap with its specimen from the suction system and securely closes the container 17. Reassess vital signs, breath sounds, and SPO2 18. Ensures the safety and comfort of the patient and that any oxygen adjuncts have been replaced, e.g., nasal cannula RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ Student Signature: _________________________________________________________ Date: ____________________ 23 MEASURING MEDICATION USING A SYRINGE STUDENT NAME: ______________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Verifies physician’s order 2. Selects and gathers the necessary equipment: a. 3 mL syringe or 1 mL TB syringe b. Medium gauge needle c. Alcohol swab d. Medication vial 3. Examines the medication vial and verifies correct medication, dosage, and expiration date 4. Calculates the proper dosage required for the ordered medication 5. Wipes the rubber cap of the medication vial with alcohol swap, inserts needle and withdraws the proper amount of medication 6. Recaps the needle using a one-handed scoop technique 7. Replaces cap on medication bottle and stores properly 8. Labels syringe with medication name and dosage 9. After dispensing medication into nebulizer, disposes of syringes and needles in the appropriate sharps container RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: ________________________________________________________ Date: _____________________ 24 INITIATION OF SMALL VOLUME NEBULIZATION (SVN) STUDENT NAME: _____________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Verifies physician’s order and reviews chart for pertinent data 2. Gathers the necessary equipment; a. Flow meter b. SVN with oxygen tubing c. Aerosol mask or mouthpiece d. Medication 3. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 4. Decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash, and then dons non-sterile gloves 5. Positions the patient sitting upright and assesses the patient’s vital signs and breath sounds 6. Assembles the equipment and aseptically places medication into the SVN 7. Sets gas flow at 8-10 L/min 8. Places mask on patient’s face or mouth piece in patient’s mouth and instructs the patient to breath normally 9. Periodically assesses the patient’s vital signs and breath sounds during therapy 10. Asks the patient to cough and evaluates sputum 11. After the medication has been nebulized, rinses the SVN with sterile water, and allows it to air dry, or discards the unit 12. Reassesses patient 13. Removes gloves and decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash 25 14. Records relevant data in patient’s chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the health care team INITIATION OF SMALL VOLUME NEBULIZATION (SVN) RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: _________________________________________________________ Date: ____________________ 26 ADMINISTRATION OF MEDICATION VIA pMDI & DPI STUDENT NAME: _____________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Verifies physician’s order and reviews chart for pertinent data 2. Gathers the necessary equipment: a. pMDI or DPI b. Spacer or Holding Chamber using pMDI 3. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 4. Washes hands using the appropriate hand-hygiene procedure and initiates standard and/or transmission based precautions 5. Positions the patient sitting upright and assesses vital signs, breath sounds, and the patient’s ability to perform procedure and follow directions pMDI: Respiratory rate less than 25 DPI: Able to inhale rapidly – inspiratory flows >60 LM 6. pMDI Warms the pMDI to hand or body temperature Assembles the apparatus, making sure there are not objects in the device that could be aspirated or obstruct outflow Holds the canister vertically and shakes it vigorously Actuates one puff into the air if the unit has not been used for 24 hours of more Attaches the spacer or holding chamber and positions it in the patient’s mouth (or places the mask over the patient’s nose and mouth) While the patient is breathing normally, actuates the pMDI and has the patient breath through the device for 3 – 7 breaths, encourages breath-holding when possible Allows 1 – 2 minutes between actuations DPI Assembles the apparatus Loads medication Instructs the patients as follows: i. Exhale normally ii. Seal lips around the mouthpiece iii. Inhale deeply and forcefully (a breath hold should be encouraged but is not essential) iv. Repeat the process until dosage is complete 27 ADMINISTRATION OF MEDICATION VIA MDI & DPI PROCEDURE Satisfactory Unsatisfactory 7. Reassesses the patient and monitors the patient for adverse reactions 9. Removes gloves and decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash 10. Ensures the safety and comfort of the patient before leaving patient's room 11. Records relevant data in patient’s chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the health care team RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: ________________________________________________________________ Date: ____________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: _________________________________________________________________ Date: ____________ 28 CHEST PHYSIOTHERAPY - POSTURAL DRAINAGE/PERCUSSION/VIBRATION STUDENT NAME: ___________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Verifies physician's order and reviews patient chart for significant findings and data 2. Identifies and gathers the necessary equipment, e.g., mechanical percussor 3. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 4. Decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash, and then dons non-sterile gloves 5. Assesses the patient’s vital signs and breath sounds 6. Places patient in appropriate postural drainage positions for targeted segments, modifying position to accommodate patient’s response 7. Provides percussion while coaching the patient to take slow deep breaths during the treatment 8. Follows percussion with vibration and instructs patient to cough 9. Repeats sequence 6-8 for additional targeted areas 10. Discontinues treatment is and notifies the proper personnel if any adverse reactions occur 11. After completing treatment, returns patient to a comfortable position and instructs and assists the patient to cough, noting any sputum production; amount, color, viscosity, and odor 29 CHEST PHYSIOTHERAPY - POSTURAL DRAINAGE/PERCUSSION/VIBRATION PROCEDURE Satisfactory Unsatisfactory 12. Reassess the patient 13. Removes gloves and decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash 14. Ensures the safety and comfort of the patient before leaving patient's room 15. Records relevant data in patient chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the heath care team RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: _________________________________________________________ Date: ____________________ 30 BEDSIDE SPIROMETRY – FORCED VITAL CAPACITY (FVC) STUDENT NAME: _____________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Verifies physician’s order and reviews chart for pertinent data 2. Gathers the necessary equipment; a. Portable spirometer b. Disposable mouth piece c. Nose clip d. 3-liter calibration syringe e. Filter (if applicable) 3. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 4. Washes hands using the appropriate hand-hygiene procedure and initiates standard and/or transmission based precautions 5. Assesses the patient’s vital signs and breath sounds 6. Assembles the equipment and enters patient’s demographic and other required information into spirometer database 7. Provides clear patient instruction and demonstration for FVC 8. Coaches patient to obtain maximum patient effort for each test trial 9. Properly applies acceptability criteria for each maneuver and selects the best FVC and FEV1 results out of 3 acceptable trials for reporting 10. Removes gloves and decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash 12. Ensures the safety and comfort of the patient before leaving patient's room 13. Records relevant data in patient’s chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the health care team 31 BEDSIDE SPIROMETRY – FORCED VITAL CAPACITY (FVC) RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: ___________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _____________________________________________________________________ _________________________________________________________________________________________________ Student Signature: _____________________________________________________ Date: _____________________ 32 INCENTIVE SPIROMETRY STUDENT NAME: ___________________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Verifies physician’s order and reviews chart for pertinent data and reviews patient chart for significant findings and data, i.e., conditions predisposing to the development of atelectasis, chest x-ray for presence and location of atelectasis 2. Identifies and gathers the necessary equipment a. Incentive spirometer 3. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 4. Washes hands using the appropriate hand-hygiene procedure and initiates standard and/or transmission based precautions 5. Verifies patient’s identity and assesses the patient’s vital signs and breath sounds 6. Determines target volume to be achieved according to patient age and height (see manufacture's insert) 7. Assembles the device (volume, flow or electronic device, patient tubing, and mouthpiece) 8. Instructs patient on how to use the device effectively, taking a slow deep breath at the appropriate flow rate; attempts to achieve target volume; performs breath-hold for at least 5-10 seconds 9. Evaluates patient technique and provides appropriate feedback 33 INCENTIVE SPIROMETRY PROCEDURE Satisfactory Unsatisfactory 10. Re-adjusts volume or flow goals as necessary to challenge the patient during the procedure. 11. Instructs the patient to perform approximately 6 - 10 breaths every hour 12. Places device within reach of the patient and reinforces instructions for patient to perform independently 13. Assess vital signs and breath sounds 14. Removes gloves and decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash 15. Ensures the safety and comfort of the patient before leaving patient's room 16. Records relevant data in patient chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the heath care team RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: _________________________________________________________ Date: ____________________ 34 POSITIVE AIRWAY PRESSURE (PAP) / POSITIVE EXPIRATORY PRESSURE (PEP) THERAPY STUDENT NAME: _____________________________________ PROCEDURE DATE: _____________ Satisfactory Unsatisfactory 1. Verifies physician’s order and reviews chart for pertinent data 2. Gathers the necessary equipment (EZ-PAP, Flutter Valve, PEP mask valve, Acapella, etc.) 3. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 4. Washes hands using the appropriate hand-hygiene procedure and initiates standard and/or transmission based precautions 5. Assesses vital signs and breath sounds 6. Positions the patient 7. Places the mask comfortably over the nose and mouth or places a nose clip on the patient if using a device with a mouthpiece 8. Instructs the patient to take a larger than normal breath, but not to TLC, and to exhale slowly 9. Observes the pressure on the manometer (if applicable) to ensure that the patient is receiving the prescribed pressure (if applicable) 10. Instructs the patient to take 10 – 20 breaths followed by 2 – 3 huff coughs, and to repeat this procedure 4 – 8 times over 10 – 20 minutes 11. Notes the quantity, color, viscosity, and odor of any sputum expectorated 12. Reassess the patient 13. Correctly removes and disposes of PPE and washes hands 35 POSITIVE AIRWAY PRESSURE (PAP) / POSITIVE EXPIRATORY PRESSURE (PEP) THERAPY STUDENT NAME: _____________________________________ PROCEDURE DATE: _____________ Satisfactory Unsatisfactory 14. Ensures the safety and comfort of the patient before leaving patient's room 15. Records relevant data in patient chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the heath care team RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: _________________________________________________________ Date: ____________________ 36 INTERMITTENT POSITIVE PRESSURE BREATHING (IPPB) THERAPY STUDENT NAME: __________________________________________________ PROCEDURE Satisfactory Unsatisfactory 1. Verifies physician's order and reviews patient chart for significant findings and data, i.e., conditions predisposing to the development of atelectasis, chest x-ray for presence and location of atelectasis 2. Identifies and gathers the necessary equipment (IPPB machine, circuit, Wright spirometer, appropriate patient interface, e.g., mouth piece, IPPB mask, mouth seal, endotracheal/tracheostomy tube adaptor, nose clip, medications bedside spirometer if FVC is not in chart,) 3. Introduces self to patient, verifies the patient’s identity, identifies the patient’s learning needs, and explains the procedure in terms the patient/family can understand 4. Washes hands using the appropriate hand-hygiene procedure and initiates standard and/or transmission based precautions 5. Assesses the patient’s vital signs and breath sounds 6. Establishes base line information from spirometry on one or more of the following: Peak Flow, VC, FEV1, FVC 7. Determines appropriate target volume to be achieved (10 – 15 ml/kg of ideal body weight) 8. Assembles equipment and ensures its proper function (pressure check) 9. Adjusts initial settings: Low pressure 10 – 15 cm H20, moderate flow 15 L/min, moderate sensitivity -1 to -2 cm H2O 10. Aseptically fills nebulizer with prescribed medication 37 INTERMITTENT POSITIVE PRESSURE BREATHING (IPPB) THERAPY PROCEDURE Satisfactory Unsatisfactory 11. Instructs the patient to insert the mouthpiece and inhale slightly until the machine triggers on (adjust sensitivity if needed) and to maintain a tight seal around the mouthpiece so that the machine can augment inspiration (applies nose clip, mouth seal, or mask as appropriate) 12. Notes the volume achieved with a spirometer and adjusts the pressure and flow until a target volume is achieved during inspiration without patient discomfort 13. Monitors the patient vital signs throughout the therapy and observes the patient for adverse outcomes, e.g., hyperventilation, gastric distention, nausea, etc. 14. After completing therapy reassess the patient vital signs and breath sounds and performs post-treatment spirometry and notes outcomes 15. Instructs patient to cough and notes any sputum production; amount, color, viscosity, and odor 16. Disassembles equipment and discards unused medication from the nebulizer, rinses it with sterile water, and allows to air dry 17. Removes gloves and decontaminates hands with an alcohol-based hand rub or performs a 15 second hand wash 18. Ensures the safety and comfort of the patient before leaving patient's room 19. Records relevant data in patient chart and appropriate departmental records, and communicates pertinent information regarding patient’s clinical status to appropriate members of the heath care team 38 INTERMITTENT POSITIVE PRESSURE BREATHING (IPPB) THERAPY RATING Satisfactory (no critical errors, corrects with some coaching or without supervision) Unsatisfactory (critical errors, requires remediation) Evaluator Signature: _______________________________________________________ Date: ____________________ Comments/Remedial Action Plan: _______________________________________________________________________ ___________________________________________________________________________________________________ ___________________________________________________________________________________________________ Student Signature: _________________________________________________________ Date: ____________________ 39 40 RET 2833 CLINIC – TASKS COMPLETION RECORD Student Name: ______________________________________________ TASK DESCRIPTION DATE Instructor Initials INSERTION OF OROPHARYNGEAL AIRWAY DURING MANUAL RESUSCITATION OROPHARYNGEAL SUCTIONING USING A TONSIL TIP SUCTION DEVICE INSERTION OF NASOPHARYNGEAL AIRWAY / NASOTRACHEAL SUCTIONING AND SPECIMEN COLLECTION ENDOTRACHEAL TUBE/TRACHEOSTOMY TUBE SUCTIONING WITH: C. SUCTION CATHETER D. CLOSED SUCTION SYSTEM DRAWING AND MEASURING MEDICATION USING A SYRINGE INITIATION OF SVN FOR AEROSOLIZATION OF MEDICATION ADMINISTRATION OF MEDICATION VIA A MDI / DPI CHEST PHYSIOTHERAPY - POSTURAL DRAINAGE / PERCUSSION / VIBRATION BEDSIDE SPIROMETRY INCENTIVE SPIROMETRY POSITIVE AIRWAY PRESSURE (PAP) / POSITIVE EXPIRATORY PRESSURE (PEP) THERAPY IPPB THERAPY ADMINISTRATION - BIRD SERIES DCE ______________________________________________________________ DATE _______________ Instructors will date and initial the Task Sheet Completion Record as the student successfully completes each task. The Task Sheet Completion Record will be collected by the instructor at the conclusion of RET 2833 Clinic 2 and placed in the student’s record. 41