REPORT OF HEALTH EVALUATION EDINBORO UNIVERSITY DEPARTMENT OF CONTINUING EDUCATION
advertisement
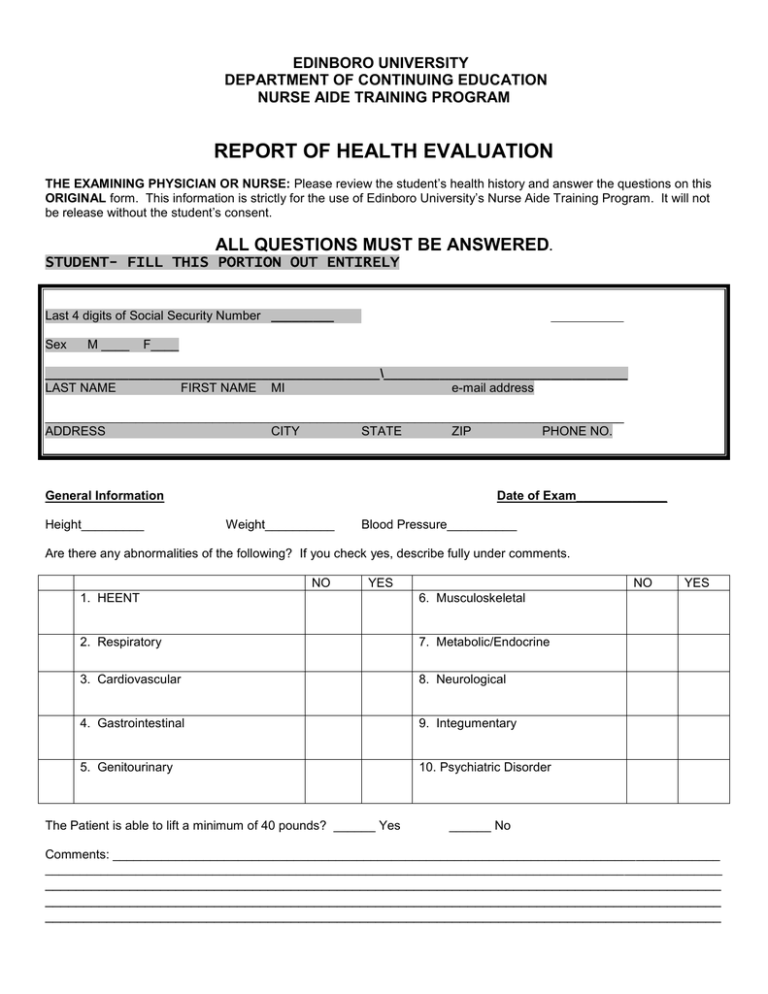
EDINBORO UNIVERSITY DEPARTMENT OF CONTINUING EDUCATION NURSE AIDE TRAINING PROGRAM REPORT OF HEALTH EVALUATION THE EXAMINING PHYSICIAN OR NURSE: Please review the student’s health history and answer the questions on this ORIGINAL form. This information is strictly for the use of Edinboro University’s Nurse Aide Training Program. It will not be release without the student’s consent. ALL QUESTIONS MUST BE ANSWERED. STUDENT- FILL THIS PORTION OUT ENTIRELY Last 4 digits of Social Security Number _________ Sex M ____ F____ ________________________________________________\___________________________________ LAST NAME FIRST NAME MI e-mail address ___________________________________________________________________________________ ADDRESS CITY STATE ZIP PHONE NO. General Information Height_________ Date of Exam_____________ Weight__________ Blood Pressure__________ Are there any abnormalities of the following? If you check yes, describe fully under comments. NO YES NO 1. HEENT 6. Musculoskeletal 2. Respiratory 7. Metabolic/Endocrine 3. Cardiovascular 8. Neurological 4. Gastrointestinal 9. Integumentary 5. Genitourinary 10. Psychiatric Disorder The Patient is able to lift a minimum of 40 pounds? ______ Yes YES ______ No Comments: _______________________________________________________________________________________ _________________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ EDINBORO UNIVERSITY DEPARTMENT OF CONTINUING EDUCATION NURSE AIDE TRAINING PROGRAM NAME ___________________________________________ EMAIL ADDRESS PHONE NUMBER __________________________ ______________________________________ XXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXX #1) TWO-STEP PPD IS REQUIRED If there has not been a Mantoux test done within the past year, the 2-step method is required. If one was done within previous 12 months, submit verification of that date, placement and result in addition to this current PPD. (If one on file in nursing office, submit current PPD.) Step #1 Date test performed: _________ R arm/ L arm _________ Initials of tester ________ Date test read: __________ Initials of reader _______ positive ____ negative____ (PPD) _____ mm of induration STEP #2 IS TO BE GIVEN 7 – 21 DAYS AFTER STEP #1 Step #2 Date test performed: _________ R arm/ L arm _________ Initials of tester ________ Date test read: __________ Initials of reader _______ positive ____ negative____ (PPD) _____ mm of induration If there is a history of a positive TB skin test in the past, attach documentation of that positive TB skin test, evaluation and recent chest x-ray results. Follow-up: Chest x-ray: Date ____________ Results __________________________ XXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXX 2) Ten Panel Urine Drug Test Date ________ Comments if positive: ________________________ _____Positive _____Negative ATTACH A COPY OF THE LAB REPORT FOR DRUG SCREEN Signature of Physician or Certified Registered Nurse Practitioner X____________________________________________________________________________ Printed Name __________________________________________________ Date __________________ Address ________________________________________________________________________________