Cultural Competence: A Systematic Review of Healthcare Provider Education Interventions
advertisement

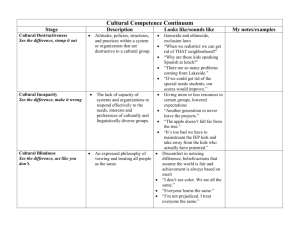
Cultural Competence: A Systematic Review of Healthcare Provider Education Interventions Mary Catherine Beach, MD, MPH Eboni G. Price, MD Tiffany L. Gary, PhD Karen A. Robinson, MSc Aysegul Gozu, MD Carole Smarth, MD Ana Palacio, MD, MPH Mollie W. Jenckes, MHS, RN Carolyn Feuerstein, BA Eric B. Bass, MD, MPH Neil R. Powe, MD, MPH, MBA Lisa A. Cooper, MD, MPH The Johns Hopkins Evidence-based Practice Center, Baltimore, MD Funded by the Agency for Healthcare Research and Quality Cultural Competence of Health Professionals • The ability of individuals to establish effective interpersonal and working relationships that supersede cultural differences 1 • Suggested to reduce disparities in healthcare for racial/ ethnic minority patients • Required by ACGME for professionalism • Little systematic evaluation of its potential 1 Cooper LA, Roter DL. in Unequal Treatment. Washington, DC: Nat’l Academies Press, 2003 Study Aim • To determine the effectiveness and costs of interventions designed to improve cultural competence of health professionals Study Design • Systematic review of all interventions to reduce disparities or improve healthcare quality for racial/ethnic minorities • Electronic Searches – MEDLINE, the Cochrane CENTRAL Register of Controlled Clinical Trials, EMBASE, and specialty databases • Hand Searches – Reference lists of all eligible articles Inclusion Criteria Exclusion Criteria • Intervention focused on cultural competence • Intervention targeted at health professionals • Adequate evaluation of intervention (pre/post or controlled trial) • Published prior to 1980 • Not in English • No original data • Meeting abstract (no full article for review) Review Process • 2 reviewers reviewed all abstracts and articles for eligibility • Differences between reviewers adjudicated • If article eligible, we – Graded article quality using previously validated, standardized forms – Abstracted data related to targeted providers and settings, curricular content, teaching methods, evaluation methods, and outcomes Synthesis/ Evidence Grading Overall Score Domains Quantity Consistency Quality Bias Objective Assessment A - Excellent >=3 Consistent >= 1 RCT >=75% studies B – Good Reasonably consistent >= 1 controlled trial >=50% Inconsistent No controlled trials >=25% C - Fair >=2 D - Poor >=1 <25% Results: Literature Search and Eligibility Electronic Databases 4309 Hand Searching 79 Retrieved 4388 Duplicates 679 Abstract Review 3709 Article Review 281 Excluded 3421 Unable to Review 7 Excluded 247 Eligible articles 34 Characteristics of Studies (N=34) n Study Design Pre/Post Control Setting 20 U.S. 14 Subjects Physicians n 29 18 Publication Years Objective Evaluation 1980-89 5 Yes 26 1990-1999 19 Intervention Description >2000 10 Complete 16 Curricular Methods and Content Methods Lectures Discussion Case Scenarios Role Play Small Group Clinical Experience Interaction with others Audio-visual Cultural Immersion n 19 17 13 12 11 10 9 9 8 Content n Specific Cultures 26 General Concepts 19 Language 10 MD-PT Interactions 8 Access 3 Racism 2 SES 2 Effects of Cultural Competence Training Benefit No Effect Mixed Harm 25 # of Studies 20 15 10 1 1 17 3 1 21 14 3 5 1 0 Knowledge Attitudes Skills Satisfaction Adherence Interventions that Improved Patient Satisfaction/ Adherence Intervention Target Duration Spanish language ED physicians 20 hours Training in attitudes that low-income AA women might bring to counseling State mandated training program including cultural competence Mental health counselors 4 hours Mental health clinics 3 days Summary of Effectiveness Level of Evidence Outcome Excellent evidence Good evidence Poor evidence No evidence Provider knowledge and attitudes Provider skills and patient satisfaction Patient adherence Impact on patient health Which types of training are most effective Costs • Costs of international travel (3 articles) – all required students to pay part or all of the costs ~ $1200 - 2000 per student • Costs of classroom instruction (2 articles) – 20 hours of Spanish-language classes for 9 physicians = $2000 (2000) – 60 hours of classroom instruction for 19 students $3000 (1994) Conclusions • Excellent or good evidence that cultural competence training can improve provider knowledge, attitudes, and skills and patient satisfaction • Poor or no evidence that cultural competence training can improve patient adherence or health outcomes • More comprehensive and rigorous studies are needed to guide education in cultural competence Limitations of Literature • Each curricular intervention was different; generalizability across studies difficult • No standard instruments for measuring cultural competence • Few studies – describe interventions well enough to permit replication – measured patient outcomes – included data on costs Implications for Future Research • Use study designs that minimize bias • Develop/ use reliable instruments to measure cultural competence • Assess outcomes objectively and include patient outcomes • Replicate existing curricula • Compare different curricular methods • Include data on costs